
Lipo Burn Capsules
This product is available solely through our 503A Compounding Pharmacy, ensuring personalized care and precision in every order. Please note that a valid prescription is required for purchase. If you do not have an account, please contact us.
Product Overview
Caffeine
Caffeine is a naturally occurring xanthine derivative used as a CNS and respiratory stimulant, or as a mild diuretic. Other xanthine derivatives include the bronchodilator theophylline and theobromine, a compound found in cocoa and chocolate. Caffeine is found in many beverages and soft drinks. Caffeine is often combined with analgesics or with ergot alkaloids for the treatment of migraine and other types of headache. Caffeine is also sold without a prescription in products marketed to treat drowsiness, or in products for mild water-weight gain. Caffeine was first approved by the FDA for use in a drug product in 1938. Clinically, it is used both orally and parenterally as a respiratory stimulant in neonates with apnea of prematurity. Caffeine reduces the frequency of apneic episodes by 30—50% within 24 hours of administration.[1] Caffeine is preferred over theophylline in neonates due to the ease of once per day administration, reliable oral absorption, and a wide therapeutic window. A commercial preparation of parenteral caffeine, Cafcit®, was FDA approved for the treatment of apnea of prematurity in October 1999, after years of availability only under orphan drug status (e.g., Neocaf). The FDA has continued the orphan drug status of the approved prescription formulation.
DHEA
Dehydroepiandrosterone (DHEA) is a C19 steroid also known as 5-androsten-3 beta-ol-17-one. DHEA and DHEAS (an active, sulfated form of DHEA), are endogenous hormones secreted by the adrenal cortex in primates and a few non-primate species in response to ACTH. DHEA is a steroid precursor of both androgens and estrogens, and thus is often called ‘the mother hormone’. Endogenous DHEA is thought to be important in several endocrine processes, but current medical use of DHEA is limited to controlled clinical trials. In 1997, Pharmadigm, Inc. received an orphan drug designation to enroll patients with thermal burns who require skin-grafting into trials using injectable DHEAS, known as PB-005. Researchers continue to investigate the role of both endogenous and exogenous DHEA in CNS, psychiatric, endocrine, gynecologic and obstetric, immune, and cardiovascular functions.[2] GeneLabs Technologies, Inc., submitted an NDA in September 2000 for its proprietary DHEA product, called prasterone (Prestara™, formerly known Aslera™ or GL-701). Prasterone appears to attentuate some symptoms of mild-to-moderate systemic lupus erythematosus (SLE) and may increase bone density based on evidence from two phase III studies in women; studies in men with SLE are ongoing. The FDA placed Prestara™ under a 6-month priority review status in October 2000; on April 19, 2001 the FDA stated that although the drug showed advantages over placebo in one study, the advantages were not statistically significant. Additional data were submitted to the FDA following a ‘not approvable’ letter on June 26, 2001. On September 2, 2002, the FDA issued an ‘approvable’ letter for the Prestara™ product, but the agency has asked for additional clinical trial data regarding the drug’s effects on bone mineral density before granting final approval for SLE. The manufacturer began a confirmatory phase III trial in early 2003; the primary endpoint will be measurement of bone mineral density of the lumbar spine; the trial is targeted for completion at the end of 2003. In October 2004, the manufacturer released information that Prestara™ therapy did not meet the primary end point in the confirmatory trial. In August 2003, Paladin Labs Inc., received orphan drug designation from the FDA for prasterone, dehydroepiandrosterone, DHEA, under the brand name Fidelin™, for adrenal insufficiency.
Exogenously administered DHEA is sold as a nutritional supplement in health and drug stores and many older individuals are using it to ‘maintain the vitality of their youth’. There is currently no objective, well-controlled, large-scale, scientific evidence to back claims that taking DHEA combats the signs or symptoms of aging, diabetes, neurologic disease, sexual dysfunction, or heart disease.[3] Some athletes abuse DHEA believing that it can enhance the body’s synthesis of testosterone; the potential action of DHEA as an anabolic steroid has lead to the prohibition of supplementation in competitive sport, even though evidence of anabolic effects in athletes is lacking.[4] DHEA is also abused by athletes in an attempt to normalize the testosterone:epitestosterone ratio. However, the sensitivity and specificity of currently available testing for athletic ‘doping’ can readily identify the presence of banned substances, including testosterone. Because of DHEA’s complex physiologic actions, more than 500 scientific articles investigating it have been published since 1993. Many of the short-term trials of DHEA to date have lacked the rigor and statistical applications needed to support therapeutic claims. Most claims will need to be confirmed by large-scale, properly conducted, and controlled studies. In 1984, the FDA banned the non-prescription (OTC) sale of exogenous DHEA due to concern over hepatotoxicity (hepatitis and hepatic tumors) as noted in animal studies. The FDA formally relegated DHEA to a Category II OTC ingredient at that time (i.e., not generally recognized as safe and effective). However in 1994, the passage of the US Dietary Supplement Health and Education Act (DSHEA) allowed DHEA to be marketed as a nutritional or dietary supplement.
Inositol
Inositol is a family of cyclic sugar alcohols consisting of nine stereoisomers of hexahydroxycyclohexane. The stereoisomers of the inositol family are myo-, scyllo-, muco-, neo-, allo-, epi-, cis-, and the enantiomers L- and D-chiro-inositol. Of these, myo-inositol and D-chiro-inositol are among the most abundant biologically active forms. The enzyme epimerase converts myo-inositol to the D-chiro-inositol isomer, maintaining organ-specific ratios of the two isomers. Physiologically, the concentration of myo-inositol is several times higher than D-chiro-inositol in most tissues.[5]
The myo-inositol derivative phosphatidylinositol is an important component of the lipid bilayer of cell membranes. Phosphatidylinositol and its phosphorylated forms act as second messengers that are involved in a host of cellular functions including membrane trafficking, autophagy, cell migration, and survival. Disruption of phosphoinositide lipid signaling is implicated in cancer, diabetes, and cardiovascular disorders.[6]
Inositol has shown clinical benefits in treating disorders associated with metabolic syndrome. Inositol supplementation has been effectively used to accelerate weight loss, reduce fat mass,[7] improve serum lipid profiles and upregulate the expression of genes involved in lipid metabolism and insulin sensitivity[8] in women with polycystic ovarian syndrome. Myo-inositol alone or in combination with D-chiro-inositol significantly reduced weight, BMI, and waist-hip circumference ratios in overweight/obese women with PCOS. Weight loss, reduction in fat mass and increase in lean mass were accelerated when inositol supplementation was accompanied by a low-calorie diet.[9] In addition, inositol supplementation was associated with lower rate of gestational diabetes and preterm delivery in pregnant women.[7] Currently, research is being performed to assess whether inositol may be used in treating various cancers.
Methionine
Methionine is a sulfur-containing branched-chain amino acid. A precursor for cellular methylation reactions, methionine plays an important role in lipid metabolism, polyamine synthesis, immune function, heavy metal chelation, and maintenance of redox balance.[10] Conversely, dietary methionine restriction in rodents increased energy expenditure, improved insulin resistance, and enhanced lipolysis and fatty acid oxidation in adipose tissue.[11]
The lipotropic effects of methionine may be attributed to its metabolite S-adenosyl methionine (SAM). SAM is synthesized from methionine via an energy-consuming reaction. SAM administered orally or by injection has been investigated as a treatment for liver diseases, osteoarthritis, and depression.[12] The benefits bestowed by SAM may be due to its role as a methyl donor in biochemical processes governing lipid homeostasis, DNA stability, gene expression, and neurotransmitter release.[13][14][15]
Methylcobalamin
Methylcobalamin, or vitamin B12, is a B-vitamin. It is found in a variety of foods such as fish, shellfish, meats, and dairy products. Although methylcobalamin and vitamin B12 are terms used interchangeably, vitamin B12 is also available as hydroxocobalamin, a less commonly prescribed drug product (see Hydroxocobalamin monograph), and methylcobalamin. Methylcobalamin is used to treat pernicious anemia and vitamin B12 deficiency, as well as to determine vitamin B12 absorption in the Schilling test. Vitamin B12 is an essential vitamin found in the foods such as meat, eggs, and dairy products. Deficiency in healthy individuals is rare; the elderly, strict vegetarians (i.e., vegan), and patients with malabsorption problems are more likely to become deficient. If vitamin B12 deficiency is not treated with a vitamin B12 supplement, then anemia, intestinal problems, and irreversible nerve damage may occur.
The most chemically complex of all the vitamins, methylcobalamin is a water-soluble, organometallic compound with a trivalent cobalt ion bound inside a corrin ring which, although similar to the porphyrin ring found in heme, chlorophyll, and cytochrome, has two of the pyrrole rings directly bonded. The central metal ion is Co (cobalt). Methylcobalamin cannot be made by plants or by animals; the only type of organisms that have the enzymes required for the synthesis of methylcobalamin are bacteria and archaea. Higher plants do not concentrate methylcobalamin from the soil, making them a poor source of the substance as compared with animal tissues.
Naltrexone HCl
Naltrexone is an oral opiate receptor antagonist. It is derived from thebaine and is very similar in structure to oxymorphone. Like parenteral naloxone, naltrexone is a pure antagonist (i.e., agonist actions are not apparent), but naltrexone has better oral bioavailability and a much longer duration of action than naloxone. Clinically, naltrexone is used to help maintain an opiate-free state in patients who are known opiate abusers. Naltrexone is of greatest benefit in patients who take the drug as part of a comprehensive occupational rehabilitative program or other compliance-enhancing program. Unlike methadone or LAAM, naltrexone does not reinforce medication compliance and will not prevent withdrawal. Naltrexone has been used as part of rapid and ultrarapid detoxification techniques. These techniques are designed to precipitate withdrawal by administering opiate antagonists. These approaches are thought to minimize the risk of relapse and allow quick initiation of naltrexone maintenance and psychosocial supports. Ultrarapid detoxification is performed under general anesthesia or heavy sedation. While numerous studies have been performed examining the role of these detoxification techniques, a standardized procedure including appropriate medications and dose, safety, and effectiveness have not been determined in relation to standard detoxification techniques.[16] Naltrexone supports abstinence, prevents relapse, and decreases alcohol consumption in patients treated for alcoholism. Naltrexone is not beneficial in all alcoholic patients and may only provide a small improvement in outcome when added to conventional therapy. The FDA approved naltrexone in 1984 for the adjuvant treatment of patients dependent on opiate agonists. FDA approval of naltrexone for the treatment of alcoholism was granted January 1995. The FDA approved Vivitrol, a once-monthly intramuscular naltrexone formulation used to help control cravings for alcohol in April 2006, and then in October 2010, the FDA approved Vivitrol for the prevention of relapse to opioid dependence after opioid detoxification.
Phentermine HCl
Phentermine is an oral sympathomimetic amine used as an adjunct for short-term (e.g., 8—12 weeks) treatment of exogenous obesity. The pharmacologic effects of phentermine are similar to amphetamines. Phentermine resin complex was approved by the FDA in 1959, but is no longer marketed in the US. Phentermine hydrochloride was FDA approved in 1973. In the mid-90s, there was renewed interest in phentermine in combination with another anorectic, fenfluramine, for the treatment of obesity and substance abuse, however, little scientific data support this practice. On July 8, 1997, the FDA issued a ‘Dear Health Care Professional’ letter warning physicians about the development of valvular heart disease and pulmonary hypertension in women receiving the combination of fenfluramine and phentermine; fenfluramine was subsequently withdrawn from the US market in fall of 1997. Use of phentermine with other anorectic agents for obesity has not been evaluated and is not recommended. In May 2011, the FDA approved a phentermine hydrochloride orally disintegrating tablet (Suprenza) for the treatment of exogenous obesity.[17]
Yohimbine HCl
Yohimbine is an oral alpha-2 blocker that is chemically related to reserpine. It is an alkaloid found in the bark of Rubiaceae and related trees, but can also be found in Rauwolfia serpentina. Yohimbine has been proposed as a treatment for erectile dysfunction (ED), however only limited evidence exist. According to ED treatment guidelines, only one small study in the published literature used acceptable efficacy outcome measures; therefore, conclusions about the clinical efficacy of yohimbine have not been established and its use in the treatment of ED is not recommended. Further, associated adverse events such as elevations of blood pressure and heart rate, increased motor activity, irritability, and tremor may limit its use.[18][19] Yohimbine has been available since before 1938.
Caffeine
Caffeine is a mild, direct stimulant at all levels of the CNS and also stimulates the heart and cardiovascular system. The related xanthine, theophylline, shares these properties and is widely used in the treatment of pulmonary disease. Both caffeine and theophylline are CNS stimulants, with theophylline exerting more dramatic effects than caffeine at higher concentrations. Caffeine also stimulates the medullary respiratory center and relaxes bronchial smooth muscle. Caffeine stimulates voluntary muscle and gastric acid secretion, increases renal blood flow, and is a mild diuretic.
While the clinical responses to caffeine are well known, the cellular mechanism of action is uncertain. Several theories have been proposed. At high concentrations, caffeine interferes with the uptake and storage of calcium by sarcoplasmic reticulum of striated muscle. While this action would explain the effects of caffeine on cardiac and skeletal muscle, it does not appear to occur at clinically achievable concentrations. Inhibition of phosphodiesterases (and subsequent accumulation of cyclic nucleotides) also does not appear to occur at clinically achievable concentrations.
Currently, it is believed that xanthines act as adenosine-receptor antagonists. Adenosine acts as an autocoid, and virtually every cell contains adenosine receptors within the plasma membrane. Adenosine exerts complex actions. It inhibits the release of neurotransmitters from presynaptic sites but works in concert with norepinephrine or angiotensin to augment their actions. Antagonism of adenosine receptors by caffeine would appear to promote neurotransmitter release, thus explaining the stimulatory effects of caffeine.Recently, a distinct syndrome has been associated with caffeine withdrawal. It is possible that the manifestations of caffeine withdrawal may be secondary to catecholamine or neurotransmitter depletion.
The following mechanisms of action are hypothesized for caffeine’s action in apnea of prematurity: 1) stimulation of the respiratory center, 2) increased minute ventilation, 3) decreased threshold to hypercapnia, 4) increased response to hypercapnia, 5) increased skeletal muscle tone, 6) decreased diaphragmatic fatigue, 7) increased metabolic rate, and 8) increased oxygen consumption. All of these actions are thought to be related to adenosine receptor antagonism.
DHEA
Endogenous DHEA is a complex hormone, and researchers still have much to discover in regards to its physiologic effects in males and females. Less is known regarding the mechanisms of action of exogenously administered DHEA.
CNS actions: Both DHEA and DHEAS may be synthesized de-novo by the central nervous system, and concentrations of DHEA and DHEAS are higher in the brain than in other organs. The two neurohormones appear to have excitatory activity at both GABA and NMDA receptors.[2]
Dermatologic actions after burn injury: Animal studies have suggested that DHEA and DHEAS expedite the re-epithelialization of donor skin-graft sites.[20]
Endocrine actions: Endogenous DHEA is synthesized by the conversion of cholesterol via CYP11A1 to pregnenolone, followed by CYP17 conversion to DHEA and then to DHEAS via dehydroepiandrosterone sulfatransferase. The synthesis of DHEA occurs exclusively in the adrenal cortex in women, while in men 10—25% of DHEA is synthesized by the testes and roughly 80% of the DHEA comes from the adrenal glands. DHEA is converted via hydrosteroid dehydrogenases and aromatase into androstenedione, testosterone, and estradiol by peripheral tissues. DHEA is of only minor importance as an androgenic substance itself. The production rate of DHEA by the body changes dramatically throughout life, typically peaking at adrenarche, the adrenal contribution to the onset of puberty. In males, DHEA serum levels are high in neonates right after birth, rapidly fall within 5 months, then begin to rise at the age of 9 years. Endogenous DHEA concentration then peaks again in males at roughly the 20th—30th years of life. In females, DHEA serum levels are high in neonates right after birth, rapidly fall within 5 months, then begin to rise at the age of 7 years. Endogenous DHEA concentration then peaks again in females at roughly the 20th and 40th year of life. DHEA levels decline steadily after the fifth decade in both males and females. DHEAS concentrations in males and females follow similar patterns. The administration of DHEA supplements results in different hormonal concentration changes in males and females; the actions are dependent on the dose, formulation and route of administration, and age of the person receiving the DHEA.[2]
Hemostasis: Inhibition of platelet aggregation by exogenous DHEA has been demonstrated in vivo in humans; DHEA either prolonged or completely inhibited the rate of arachidonate-stimulated platelet aggregation after 14 days of administration. The degree of inhibition of platelet aggregation was noted to be time and dose dependent.[21]
Immunologic actions: Because SLE occurs more frequently in women than men and because SLE is known to worsen during pregnancy, a hormonal etiology is suspected for this disease. DHEA up-regulates interleukin-2 (IL-2) production by T-lymphocytes in murine lupus models and reverses the clinical autoimmune disease. Lower endogenous levels of DHEA and DHEAS have been noted in both male and female patients with lupus at the time of diagnosis. Chronic corticosteroid treatment, which may cause adrenal atrophy, contributes to reduced DHEA levels in these patients. Supplementation of DHEA in SLE may augment immune system activity and potentially offset the undesired effects of chronic corticosteroid use in these patients.[22] Exact mechanisms of DHEA on immune function are not yet clear. DHEA has been shown to increase the numbers of natural killer cells in aging women. Serum DHEA levels are observed to be reduced in patients with AIDS or age-related immunodeficiency, suggesting that DHEA may serve as a marker of the integrity of the immune system. No studies to date have shown that DHEA supplementation augments currently available therapies for AIDS.[2]
Inositol
Structurally, all inositol stereoisomers are 6-carbon sugar alcohols with the same molecular formula as glucose (C6H12O6). Myo-inositol and D-chiro-inositol have insulin-mimetic effects. Inositol administration in diabetic rodents, rhesus monkeys, and humans lowers post-prandial blood glucose levels and improves insulin sensitivity.[23][24][25] These benefits may be attributed to the effects of inositol on the insulin signaling pathway. Stimulating the insulin receptor activates the phosphatidylinositol-3-kinase (PI3K) pathway. Phosphorylated forms of phosphatidylinositol act as second messengers that lead to downstream activation of Akt. Akt inactivates the enzyme glycogen synthase kinase-3, enhancing glycogen synthase activity. This increases translocation of the glucose transporter (GLUT4) to the surface of skeletal muscle cells, increasing glucose uptake and lowering blood glucose levels.[26]
Excess circulating glucose is often deposited as fat in the liver and around visceral organs. Dietary supplementation with inositol reduced weight gain and lipid accumulation in the liver of rats.[27][28][29] Inositol-mediated activation of PI3K/Akt signaling is believed to play a role in hepatic lipid metabolism and gluconeogenesis. Inositol also affects transcription of SREBP-1 and PPAR-α – genes involved in fatty acid synthesis, oxidation, and lipid transport.
Methionine
An essential sulfur-containing amino acid, methionine undergoes transmethylation reactions to generate metabolic by-products including S-adenosyl methionine (SAM) and homocysteine. SAM is a universal methyl group donor that serves as a co-factor in numerous cellular and physiological processes including lipid homeostasis. By donating its methyl group, SAM is converted first to S-adenosyl homocysteine (SAH) and then to homocysteine. As a methyl donor, SAM contributes to the formation of phosphatidylethanolamine and subsequently to phosphatidylcholine. In the liver, phosphatidylcholine is packaged into very low-density lipoproteins (VLDL) and transported to other tissues. Inadequate levels of SAM in the liver disrupts VLDL assembly and leads to hepatic accumulation of triglycerides or fatty liver.[30]
By promoting DNA methylation SAM plays a crucial role in epigenetic regulation. Methylation near gene promoters is a well-known mechanism of transcriptional repression. Therefore, SAM may act as a sensor for cellular nutrient status and epigenetically alter the expression of genes influencing appetite, glucose metabolism, and lipogenesis.[31][32] SAM also functions as a methyl donor in the synthesis of creatine – a high-energy molecule known to improve exercise.[33]
Methylcobalamin
Vitamin B12 is used in the body in two forms, methylcobalamin and 5-deoxyadenosyl cobalamin. The enzyme methionine synthase needs methylcobalamin as a cofactor. This enzyme is involved in the conversion of the amino acid homocysteine into methionine which is, in turn, required for DNA methylation. The other form, 5-deoxyadenosylcobalamin, is a cofactor needed by the enzyme that converts L-methylmalonyl-CoA to succinyl-CoA. This conversion is an important step in the extraction of energy from proteins and fats. Furthermore, succinyl CoA is necessary for the production of hemoglobin, the substance that carries oxygen in red blood cells.
Vitamin B12, or methylcobalamin, is essential to growth, cell reproduction, hematopoiesis, and nucleoprotein and myelin synthesis. Cells characterized by rapid division (epithelial cells, bone marrow, myeloid cells) appear to have the greatest requirement for methylcobalamin. Vitamin B12 can be converted to coenzyme B12 in tissues; in this form it is essential for conversion of methylmalonate to succinate and synthesis of methionine from homocysteine (a reaction which also requires folate). In the absence of coenzyme B12, tetrahydrofolate cannot be regenerated from its inactive storage form, 5-methyl tetrahydrofolate, resulting in functional folate deficiency. Vitamin B12 also may be involved in maintaining sulfhydryl (SH) groups in the reduced form required by many SH-activated enzyme systems. Through these reactions, vitamin B12 is associated with fat and carbohydrate metabolism and protein synthesis. Vitamin B12 deficiency results in megaloblastic anemia, GI lesions, and neurologic damage (which begins with an inability to produce myelin and is followed by gradual degeneration of the axon and nerve head). Vitamin B12 requires an intrinsic factor-mediated active transport for absorption, therefore, lack of or inhibition of intrinsic factor results in pernicious anemia.
Naltrexone HCl
Like naloxone, naltrexone is a competitive antagonist at opiate receptors mu, kappa, and delta. Opiate receptors have been reclassified by an International Union of Pharmacology subcommittee as OP1 (delta), OP2 (kappa), and OP3 (mu). Naltrexone can either displace opiate agonists from binding at these receptors or prevent opiate binding. Naltrexone does not antagonize the effects of non-opiates such as cocaine, ethanol, amphetamines, barbiturates, or benzodiazepines. Blockade of opiate receptors by naltrexone is a competitive phenomenon and results in elimination of the euphoric effect of opiates. At usual opiate concentrations, naltrexone’s greater affinity for the receptor prevents the binding of the opiate agonist to the receptor. However, when opiate concentrations are extremely high, the opiate can displace naltrexone, and respiratory depression and/or death is possible. Although naltrexone itself may possess some agonistic properties, these are minor compared to its potent antagonistic actions. Naltrexone is 17-times more potent than nalmorphine and twice as potent as naloxone. In patients who are physically dependent on opiates, naltrexone will precipitate an opiate withdrawal syndrome. Naltrexone use is not associated with tolerance or dependence, therefore, withdrawal from naltrexone does not occur. When co-administered with opiate agonists, naltrexone blocks the physical dependence to morphine, heroin, and other opiate agonists. Depending on the dose, the clinical effects of naltrexone can persist for up to 72 hours.
Endogenous opiods such as beta-endorphins and enkephalins may play an important role in alcoholism. An opioid reward system mediated by mu- and delta-receptors and an opposing aversions system mediated by kappa-receptors must be in balance to maintain a neutral state in regards to the development of addiction. Several therories regarding alcohol addiction and the function of endongeous opioids exist. All of these therories are based on an imbalance in favor of the endongenous reward pathways due to alcohol. Naltrexone inhibits the effects of endogenous opioids and decreases the positive or reward pathways associated with alcoholism. Naltrexone is not aversive therapy and will not produce a disulfiram-like reaction if opiates or ethanol are ingested while receiving naltrexone.
Phentermine HCl
Limited data are available in reference texts regarding the mechanism of action of this drug. Phentermine is an analog of methamphetamine. Similar to the amphetamines, phentermine increases the release of norepinephrine and dopamine from nerve terminals and inhibits their reuptake. Thus, phentermine is classified as an indirect sympathomimetic.[34] Other effects include a weak ability to dose-dependently raise serotonin levels, although the effect on serotonin occurs is less potent than that of methamphetamine itself.[35] Clinical effects include CNS stimulation and elevation of blood pressure. Appetite suppression is believed to occur through direct stimulation of the satiety center in the hypothalamic and limbic region.
Tolerance to the anorexiant effects of phentermine usually develops within a few weeks of starting therapy. The mechanism of tolerance appears to be pharmacodynamic in nature; higher doses of phentermine are required to produce the same response. When tolerance develops to the anorexiant effects, it is generally recommended that phentermine be discontinued rather than the dose increased.
Yohimbine HCl
The exact mechanism of action of yohimbine in the treatment of erectile dysfunction (ED) has yet to be determined; there are few data which support its role in ED. It is believed that yohimbine exerts its effects by blocking central alpha-2 receptors thereby producing an increase in sympathetic drive secondary to an increase in norepinephrine release and in firing rate of cells in the brain noradrenergic nuclei. This activity increases penile blood inflow, decreases penile blood outflow, or both, which causes erectile stimulation without increased sexual desire. Yohimbine-mediated norepinephrine release at the level of the corporeal tissues may also be involved as well as other neurotransmitters (e.g., dopamine and serotonin). Other actions of yohimbine include a stimulant effect on mood and an increase in blood pressure at higher doses. At high doses, yohimbine may nonselectively inhibit monoamine oxidase (MAO). Mild antidiuretic actions may also be present possibly due to release of antidiuretic hormone.
Caffeine
Caffeine with sodium benzoate injection is not recommended for use in premature neonates because the benzoate may displace bilirubin and induce kernicterus. Elevated serum concentrations of benzoate, similar to benzyl alcohol, have also been associated with neurological disturbances, hypotension, gasping respiration, and metabolic acidosis (i.e., ‘gasping syndrome’) in neonates.[36] Clinicians should use Cafcit, which does not contain sodium benzoate, or use an extemporaneously compounded caffeine citrate injection in newborns and premature neonates. The safety and efficacy of the prescription use of caffeine in neonates and infants for longer than 12 days, prophylaxis of sudden infant death syndrome (SIDS), or for use prior to extubation in mechanically ventilated infants has not been established.[37]
The OTC use of caffeine products is not recommended in children under the age of 12 years.
Caffeine is a central nervous system stimulant. Caffeine should be used cautiously in patients with anxiety disorders and/or panic disorder because it can aggravate these conditions. Patients suffering from insomnia should not consume caffeine, nor should caffeine be consumed prior to retiring because it can cause insomnia. In overdoses, caffeine has been associated with seizures and it should be prescribed cautiously to those patients with a seizure disorder.
Caffeine should be used cautiously in those patients, including neonates, with cardiac disease. Caffeine can stimulate the force of contraction and can increase heart rate. It may increase left ventricular output and stroke volume. Patients who have angina or a history of cardiac arrhythmias should not receive or should minimize their intake of caffeine. Caffeine should not be taken in the first few days—weeks after a myocardial infarction. Patients with hypertension should minimize their intake of caffeine.
Caffeine should be used cautiously in those with hepatic disease or hepatic impairment. Caffeine clearance may be delayed, leading to toxicity. Renal impairment or renal failure may also delay caffeine clearance. It should be noted that caffeine elimination is more dependent on renal clearance in premature neonates and term neonates than in older infants or adults, due to the underdeveloped hepatic metabolism and renal elimination of drugs in general. Thus monitoring of serum caffeine concentrations is recommended in neonates or premature neonates, especially those with renal or hepatic impairment.
Although the effects are mild, caffeine can either raise or decrease blood sugar; use with caution in patients with diabetes mellitus. In clinical studies reported in the literature, cases of hypoglycemia and hyperglycemia have been observed in neonates receiving caffeine citrate. Therefore, blood glucose may need to be periodically monitored in infants receiving caffeine citrate.[37]
Patients with thyroid disease, especially hyperthyroidism, should not receive or should minimize their intake of caffeine. The stimulatory effects of caffeine can be augmented in hyperthyroidism.
In neonates, there are reports in the literature suggesting a possible association between the use of methylxanthines like caffeine and the development of necrotizing enterocolitis. In a clinical trial (n = 85 neonates) evaluating the use of caffeine citrate in apnea of prematurity, necrotizing enterocolitis was reported in 6 patients, 5 of whom were administered caffeine. Three of the infants died. In a much larger clinical trial (n = 2,000 neonates) evaluating the use of caffeine citrate in apnea of prematurity, necrotizing enterocolitis was not more common in caffeine treated patients compared to placebo. Preterm neonates treated with caffeine should be monitored for the development of gastric side-effects (i.e., abdominal distension, vomiting, bloody stools, and lethargy).[37][38] Caffeine can stimulate gastric secretions and may aggravate gastroesophageal reflux disease (GERD). Clinical trial data are conflicting regarding the limitation of caffeine as an effective strategy to control GERD symptoms; however, recommended lifestyle modifications for patients with GERD often include moderation of caffeine intake.[39]
Caffeine citrate is used for neonatal apnea so concerns for teratogenicity are not relevant when administered to infants, however, when 50 mg/kg of sustained-release pellets were administered to pregnant mice during the period of organogenesis, a low incidence of cleft palate and exencephaly have been noted in the fetuses.[37] Caffeine easily crosses the placenta; fetal blood and tissue concentrations approximate maternal concentrations. There are no large, well-controlled studies of caffeine administration in pregnant women; it is generally recommended that the intake of caffeine-containing beverages, like coffee, teas, and sodas, be limited in pregnancy (usually no more than 1 to 2 caffeine-containing beverages/day) or avoided if possible. Caffeine-containing medications should likewise, be limited to use only when absolutely necessary. Low to moderate caffeine intake does not appear to increase the risk of congenital malformation, spontaneous abortion, pre-term birth or low birth weight. The association between high daily intake (more than 500 mg/day) of caffeine and increased rates of low birth weight, spontaneous abortion, difficulty in getting pregnant or infertility is still controversial, as some studies have not controlled for concomitant cigarette smoking.[40] There are no adequate and well-controlled studies of caffeine administration in pregnant women. Neonatal arrhythmias (e.g., tachycardia, premature atrial contractions) and tachypnea have been reported when caffeine was consumed during pregnancy in amounts > 500 mg/day; caffeine withdrawal after birth may account for these symptoms.[41]
Although the American Academy of Pediatrics has considered the use of mild to moderate use of caffeinated beverages to be compatible with lactation, mothers who are breast-feeding should limit their intake of caffeinated beverages if possible.[42] Caffeine-containing drug-products should be used cautiously during lactation due to their high caffeine contents. Mothers who are breast-feeding infants who have been prescribed caffeine for apnea should generally avoid additional caffeine use.[37] The CYPP450 hepatic metabolism of caffeine is inhibited in infants who are breastfed; formula feeding does not appear to affect the pharmacokinetics of caffeine in infants.[43] Peak caffeine milk levels usually occur within 1 hour after the maternal ingestion of a caffeinated beverage; with milk: plasma ratios of 0.5 to 0.7 reported.[44][45] Although only small amounts are secreted in breast milk, caffeine can accumulate in the neonate if maternal ingestion is moderate to high. Higher caffeine intake (more than 500 mg/day) by a nursing mother may cause irritability or poor sleeping patterns in the infant who is breast-feeding.[46] Consider the benefits of breast-feeding, the risk of potential infant drug exposure, and the risk of an untreated or inadequately treated condition.
Tobacco smoking (cigarettes) has been shown to increase the clearance of caffeine. Passive smoke exposure may also cause an increase in caffeine clearance. This may help to explain why tobacco smokers often have concomitantly high caffeine intakes. Tobacco smoke contains hydrocarbons that induce hepatic CYP450 microsomal enzymes. Because the effect on hepatic microsomal enzymes is not related to the nicotine component of tobacco, sudden smoking cessation may result in a reduced clearance of caffeine, despite the initiation of nicotine replacement. Caffeine dosage may need to be reduced at the cessation of smoking.
Caffeine can usually be ingested in normal amounts found in food or beverages (e.g., coffee) in the elderly; however, geriatric patients should be aware of the effects of caffeine on sleep and other physiologic functions, such as urination. Excessive caffeine intake, such as intake of non-prescription caffeine dietary supplements/medicines, should generally be avoided, as excessive use can cause tremor, insomnia, palpitations, and gastrointestinal complaints. Because caffeine is an ingredient in some non-prescription products, patients should be advised to read labels carefully or check with their prescriber or pharmacist if they are unsure if the medication contains caffeine.[47]
Caffeine intake should be limited along with MAOI therapy.
DHEA
Your health care provider needs to know if you have any of these conditions: breast cancer (men or women); cancer of the lining of the uterus (endometrial cancer); diabetes or high blood sugar; immune system problems; infertility; liver disease; post-menopause; prostate cancer or an enlarged prostate gland; rheumatoid arthritis; uterine cancer; vaginal bleeding or menstrual problems; vaginal cancer; an unusual or allergic reaction to progesterone, DHEA, soy, other medicines, foods, dyes, or preservatives; pregnant or trying to get pregnant; breast-feeding. Visit your doctor or health care professional for regular checks on your progress. Women should inform their doctor if they wish to become pregnant or think they might be pregnant. There is a potential for serious side effects to an unborn child. DHEA use is banned in competitive sports. Both college (NCAA) and olympic (USOC) committees do not allow DHEA use among athletes.
NOTE: DHEA has not yet been evaluated by the Food and Drug Administration. Nutritional supplement products containing DHEA are not intended to diagnose, treat, cure, or prevent any disease. Consumers should also be informed that rigid quality control standards are not required for nutraceuticals and substantial variability can occur in both the potency and the purity of these products.
Dehydroepiandrosterone (free and sulfate) test systems measure dehydroepiandrosterone (DHEA) and its sulfate (DHEAS) in urine, serum, plasma, and amniotic fluid. These measurements are used in the diagnosis and treatment of DHEA-secreting adrenal cancers. It is unclear at this time if supplementation with DHEA would result in false-positives of these tests.
The effect of DHEA on hormone-dependent tumors in males and females is unknown. Many hormonal agents with androgenic or estrogenic activity are contraindicated for use in persons with various hormonally-dependent neoplasms. Some data suggests an association between elevated endogenous DHEA and DHEAS serum concentrations and the development of breast cancer andovarian cancer in women. As with other hormones, DHEA supplementation in a woman with undiagnosed abnormal vaginal bleeding, endometrial cancer, endometrial hyperplasia, uterine cancer, or vaginal cancer is not recommended. DHEA may stimulate the growth of cancerous tissue and should not be used in male patients with either breast or prostate cancer. Male patients with symptoms of prostatic hypertrophy or erectile dysfunction that have not been medically evaluated should not take DHEA supplements. Because the incidence of some hormonally-dependent cancers naturally increases with age, “andropausal” men and post-menopausal women should approach DHEA supplementation with caution. It is recommended that a qualified healthcare prescriber’s recommendations be sought prior to DHEA supplementation.[48] Benefit versus risk should be determined individually. Women taking DHEA should receive an annual clinical breast examination and pelvic examination and regular mammograms as recommended by their healthcare professional. Men taking DHEA should receive annual physical examinations, including prostate examination or PSA levels, as recommended by their healthcare provider.
Dehydroepiandrosterone, DHEA is contraindicated for use in children <= 18 years of age. Because endogenous DHEA, DHEAS, and androstenedione serum concentrations are related to the onset of puberty, there is concern that the use of DHEA supplements in children or adolescents would interfere with natural growth and sexual maturation. Females of childbearing age with infertility due to hyperandrogenism or chronic anovulation should not take DHEA supplements. The relationship of DHEA and DHEAS to ovulation and fertility is complex and still poorly understood. However, women with hirsutism and infertility or polycystic ovary syndrome (PCOS) are commonly found to have elevated endogenous DHEA or DHEAS serum concentrations on assay.[49] Women with higher serum levels of endogenous DHEAS and who are receiving fertility treatments have been noted to have higher rates of ovarian hyperstimulation syndrome (OHSS) associated with their treatments. DHEA may also induce changes in the normal menstrual cycle in women of childbearing age. Dehydroepiandrosterone, DHEA should be considered a pregnancy category X drug, similar to other androgenic hormones. Studies of the role of endogenous fetal and maternal DHEA in pregnancy indicate that the ratio of DHEA or DHEAS to other hormones in the serum or placenta may influence the processes of fetal development, parturition, and labor. Endogenous DHEA and DHEAS appear to be important in the functional development of the adrenal cortex and other endocrine activities in the fetus; it is assumed that exogenous DHEA supplementation to a pregnant woman could potentially have deleterious effects on fetal development or viability. The androgenic effects of DHEA could potentially result in masculinization of a female fetus. No controlled trials of DHEA in primate or human gestation exist. Do not administer DHEA to a pregnant woman. DHEA is a hormone and should not be supplemented in a lactating woman who is breast-feeding her infant. Most hormones are excreted in breast milk. Like other androgenic hormones, it is possible that DHEA could inhibit lactation. It is unknown what effect DHEA would have on the breast-feeding infant. Dehydroepiandrosterone, DHEA should be considered contraindicated for use in patients with hepatic disease, hepatitis,hepatocellular cancer, or jaundice. In 1984, the FDA banned the non-prescription (OTC) sale of DHEA due to concern over its ability to cause hepatotoxicity. DHEA supplements are now able to be sold as "nutritional supplements" secondary to the US Dietary Supplement Health and Education Act (DSHEA) of 1994, and are no longer regulated as drugs outside of clinical trials. Transient drug-induced hepatitis has been reported in association with the use of DHEA nutritional supplements. Because both estrogens and androgens may exacerbate acute intermittent or variegate hepatic porphyria, DHEA, which has androgenic actions, should be used with caution in patients with these diseases. Treatment of patients with diabetes mellitus with DHEA is currently not warranted. The role of endogenous DHEA in relationship to insulin resistance is not clear. DHEA and DHEAS may not be mediators of insulin action. Long-term trials evaluating the effectiveness and safety of exogenous DHEA supplementation in patients with diabetes are currently unavailable. Patients with diabetes mellitus who are pursuing the use of DHEA supplements should see a qualified health care professional.[50] DHEA treatment of patients with human immunodeficiency virus (HIV) infection should be approached with caution. DHEA may possess immunomodulating effects, perhaps by enhancing the secretion of IL-2 from activated T cells as demonstrated in murine models. While this suggests that DHEA may play a role in the function of the immune system, the role of DHEA supplementation in the treatment of human HIV infection, especially acquired immunodeficiency syndrome (AIDS), has not yet been determined. Safety and efficacy have not been established.[51] Most non-essential hormones are discontinued several weeks prior to major surgery where feasible. DHEA may inhibit platelet aggregation, an effect that may be important to consider during surgical procedures. The decision of when to resume DHEA after surgery would be based on the perceived additional risk from DHEA use and the need for DHEA therapy. Soy oil is the raw product from which many DHEA supplements are manufactured. Cholesterol from soy oil is converted into DHEA. DHEA products should be used cautiously in patients with a history of allergies to soy-containing foods or who exhibit immediate-type soya lecithin hypersensitivity. One of the functions of endogenous DHEA is to inhibit the enzyme glucose-6-phosphate dehydrogenase. Use DHEA with caution in patients with G6PD deficiency. Prasterone (DHEA) should be used with caution in patients with bipolar disorder. One case report exists of the appearance of mania in a predisposed patient consuming large doses of a DHEA supplement on a routine basis. Until more information is known, clinicians should be aware that emotional lability or changes in mood may occur in selected patients. Methylcobalamin Who should not take this medication? Patients with early hereditary optic nerve atrophy, cyanocobalmin hypersensitivity, and those who are pregnant. Your health care provider needs to know if you have any of these conditions: kidney disease; Leber's disease; megaloblastic anemia; an unusual or allergic reaction to methylcobalamin, cobalt, other medicines, foods, dyes, or preservatives; pregnant or trying to get pregnant; breast-feeding. Methylcobalamin is contraindicated in patients with methylcobalamin hypersensitivity or hypersensitivity to any of the medication components. Methylcobalamin is also contraindicated in patients with cobalt hypersensitivity because methylcobalamin contains cobalt. In the case of suspected cobalt hypersensitivity, an intradermal test dose should be administered because anaphylactic shock and death have followed parenteral administration of methylcobalamin. Methylcobalamin should not be used in patients with early hereditary optic nerve atrophy (Leber's disease). Optic nerve atrophy can worsen in patients whose methylcobalamin levels are already elevated. Hydroxocobalamin is the preferred agent in this patient population (see separate monograph in Less Common Drugs). Most formulations of methylcobalamin injection contain benzyl alcohol as a preservative. Benzyl alcohol may cause allergic reactions. Methylcobalamin injections should be used cautiously in those patients with benzyl alcohol hypersensitivity. Methylcobalamin, vitamin B12 preparations containing benzyl alcohol should be avoided in premature neonates because benzyl alcohol has been associated with 'gasping syndrome,' a potentially fatal condition characterized by metabolic acidosis and CNS, respiratory, circulatory, and renal dysfunction. Vitamin B12 deficiency can suppress the symptoms of polycythemia vera. Treatment with methylcobalamin or hydroxocobalamin may unmask this condition. Folic Acid, vitamin B9 is not a substitute for methylcobalamin, vitamin B12 deficiency, although it may improve vitamin B12 megaloblastic anemia. However, exclusive use of folic acid in treating vitamin B12 deficient megaloblastic anemia could result in progressive and irreversible neurologic damage. Before receiving folic acid or methylcobalamin, patients should be assessed for deficiency and appropriate therapy started concurrently. The intranasal formulations are not approved to treat acute B12 deficiency; all hematologic parameters should be normal before beginning the methylcobalamin intranasal formulations. Concurrent iron-deficiency anemia and folic acid deficiency may result in a blunted or impeded response to methylcobalamin therapy. Certain conditions may blunt or impede therapeutic response to methylcobalamin therapy. These include serious infection, uremia or renal failure, drugs with bone marrow suppression properties (e.g., chloramphenicol), or concurrent undiagnosed folic acid or iron deficiency anemia. The mechanism appears to be interference with erythropoiesis. Patients with vitamin B12 deficiency and concurrent renal or hepatic disease may require increased doses or more frequent administration of methylcobalamin. Clinical reports have not identified differences in responses between elderly and younger patients. Generally, dose selection for elderly patients should be done with caution. Elderly patients tend to have a greater frequency of decreased hepatic, renal, or cardiac function, and also have concomitant disease or receiving other drug therapy. Start with doses at the lower end of the dosing range. Naltrexone HCl Naltrexone is contraindicated in patients with hypersensitivity to naltrexone or any components of the commercially available product. Naltrexone is incorporated in 75:25 polylactide-co-glycolide (PLG) at a concentration of 337 mg of naltrexone per gram of microspheres. The diluent is composed of carboxymethylcellulose sodium salt, polysorbate 20, sodium chloride, and water for injection. Naltrexone should also not be used in patients with a known hypersensitivity to naloxone or nalmefene because these three drugs are all structurally similar. The use of naltrexone in patients with hepatic disease should be carefully considered due to the hepatotoxic effects of naltrexone and the potential for decreased clearance of naltrexone. Naltrexone does not appear to be hepatotoxic at recommended doses. However, the margin between a safe dose and a hepatotoxic dose appears to be five-fold or less. There may be a higher risk of hepatocellular injury with single doses above 50 mg, and use of higher doses and extended dosing intervals should balance the possible risks against the probable benefits. There are reports of hepatitis and significant hepatic dysfunction in association with exposure to naltrexone oral tablets and parenteral naltrexone. In patients treated with naltrexone tablets or injection who presented with elevated transaminases, other potential causes were often identified, including pre-existing alcoholic liver disease, hepatitis B and/or C infection, and concomitant usage of other potentially hepatotoxic drugs. Opioid withdrawal does not typically manifest as clinically significant hepatic dysfunction, however, abruptly precipitated opioid withdrawal may lead to systemic sequelae including acute liver injury. Warn patients of the potential risk of hepatic injury and advise them to seek medical attention if they experience symptoms of acute hepatitis. Discontinue use of naltrexone if signs/symptoms of acute hepatitis occur.[52][53][54] Depression, suicide, attempted suicide and suicidal ideation have been reported in patients receiving naltrexone for the treatment of opioid dependence. No causal relationship has been demonstrated. In the literature, endogenous opioids have been theorized to contribute to a variety of conditions. Monitor alcohol and opioid dependent patients, including those taking naltrexone, for the development of depression or suicidal thinking. Inform families and caregivers of patients being treated with naltrexone to monitor patients for the emergence of symptoms of depression or suicidality, and to report such symptoms to the patient’s healthcare provider.[54] Naltrexone is contraindicated in patients who are receiving opioid analgesics, partial opiate agonists (e.g., buprenorphine), those with current physiologic opioid dependence, and those in acute opioid withdrawal. Administration of naltrexone to these patients may precipitate an abrupt withdrawal severe enough to require hospitalization, and in some cases management in the intensive care unit. To prevent precipitation of withdrawal, patients should be opioid-free (including tramadol) for a minimum of 7—10 days prior to initiation of naltrexone. When transitioning from buprenorphine or methadone, patients may be vulnerable to precipitation of withdrawal symptoms for up to two weeks. In every case, be prepared to manage withdrawal symptomatically with non-opioid medications because there is no completely reliable method for determining whether a patient has had an adequate opioid-free period. Since the absence of an opiate drug in the urine is often not sufficient proof that a patient is opiate-free, a naloxone challenge should be done if there is any question of occult opioid dependence. A naloxone challenge test may be helpful; however, a few case reports have indicated that patients may experience precipitated withdrawal despite having a negative urine toxicology screen or tolerating a naloxone challenge test (usually in the setting of transitioning from buprenorphine treatment). Make patients aware of the risks associated with precipitated withdrawal and the need to give an accurate account of last opioid use. A positive reaction to the naloxone challenge predicts a similar response to naltrexone. Use of naltrexone is contraindicated in an individual who fails the naloxone challenge test or who has a positive urine test for opioids.The naloxone challenge can be repeated in 24 hours. Assess patients treated for alcohol dependence for underlying opioid dependence and for any recent use of opioids prior to initiation of treatment with naltrexone. Precipitated opioid withdrawal has been observed in alcohol-dependent patients in circumstances where the prescriber had been unaware of the additional use of opioids or co-dependence on opioids.[52][53][54] If a painful procedure such as surgery is planned, then naltrexone should be discontinued 72 hours prior to the procedure. Patients should be abstinent from opiate analgesia for at least 7 days before restarting naltrexone. Naltrexone treated patients who require emergent opiate analgesia may require the administration of large opiate doses to provide adequate pain control, which may increase the risk of deep or prolonged respiratory depression. A rapidly acting opiate agonist is preferred for emergent analgesia to limit the duration of respiratory depression. Non-opiate receptor mediated actions (i.e., histamine-mediated) may occur with the use of opiates and should be expected (e.g., facial swelling, itching, generalized erythema or bronchoconstriction). Other alternatives for emergent analgesia in patients taking naltrexone include the use of regional analgesia, conscious sedation, non-opiate analgesics, or general anesthetics. Attempts to overcome the antagonistic effects of naltrexone with large doses of an opiate agonist by patients maintained on naltrexone may result in potential for overdose or poisoning that may be fatal; cases of opioid overdose with fatal outcomes have been reported in patients after discontinuing treatment. Despite a prolonged pharmacologic effect, the blockade produced by naltrexone is surmountable. As the naltrexone blockade wanes and eventually dissipates, patients may respond to lower doses of opioids than previously used, potentially resulting in life-threatening opioid intoxication (respiratory compromise or arrest, circulatory collapse, etc.) if the patient uses previously tolerated doses of opioids. Patients are at particular risk at the end of the dosing interval, after missing a scheduled dose or after discontinuing naltrexone treatment. Patients should be informed of the serious consequences of attempting to overcome the opiate blockade and that they may be more sensitive to lower doses of opiate agonists once naltrexone therapy is stopped. Advise patients to inform family members and those closest to them of this increased sensitivity and risk of overdose.[52][53][54] Naltrexone and its major active metabolite are excreted primarily by the kidney. Use caution in administering naltrexone to patients with renal impairment. Pharmacokinetic parameters of naltrexone given intramuscularly are essentially unchanged in patients with a creatinine clearance of 50—80 ml/minute. The disposition of naltrexone in patients with moderate to severe renal impairment has not been evaluated. Dosage adjustments may be necessary in patients with renal dysfunction. Naltrexone is classified as FDA pregnancy risk category C. There are no adequate and well-controlled studies in pregnant women. In some individuals, opiate antagonists have been associated with a change in baseline levels of some hypothalamic, pituitary, adrenal, or gonadal hormones, although the clinical significance is not known. In rat studies, there was an increase in early fetal loss and pseudopregnancy, and a decrease in pregnancy rate. There was no evidence of teratogenicity; however, rats do not form a significant amount of the major human metabolite, 6-B-naltrexol; therefore, the potential reproductive toxicity of 6-B-naltrexol in rats is not known. There were small increases in the numbers of testicular mesotheliomas in male rats and vascular tumors in female rats during a 2-year carcinogenicity study; however, no evidence of carcinogenicity was observed in mice.[52] When considering the use of naltrexone during pregnancy for relapse prevention in alcohol or opiate dependence, the risks to the fetus of continued substance abuse by the mother should be weighed against the potential adverse effects from fetal exposure to naltrexone. Drug therapy should be considered only if supportive substance abuse prevention measures are ineffective. The effects of naltrexone during labor and delivery are unknown. According to the manufacturer, naltrexone and its metabolite are excreted into human milk, and a decision should be made to discontinue breast-feeding or discontinue naltrexone, taking into consideration the importance of the drug to the mother. Animal studies have shown the potential for tumorigenicity.[52] No reports describing the use of naltrexone during breast-feeding are available. According to the American Academy of Pediatrics (AAP), the maternal ingestion of large amounts of ethanol or opiates can cause adverse effects in the nursing infant.[55] If supportive substance abuse prevention measures are ineffective, the risks to the nursing infant of continued ethanol or opiate abuse by the mother should be weighed against the potential for adverse drugs effects when determining whether to use naltrexone as a substance abuse deterrent during breast-feeding. The safe use of naltrexone in neonates, infants, children, and adolescents < 18 years has not been established. Naltrexone may cause dizziness (see Adverse Reactions). Tell patients about the importance of not driving or operating machinery until they know how this medicine will affect them. Administer the extended-release injectable suspension of naltrexone cautiously to patients with thrombocytopenia, coagulopathy, or other bleeding disorders. Patients with thrombocytopenia, vitamin K deficiency, a coagulopathy (e.g., hemophilia), or receiving anticoagulant therapy should be monitored closely when given intramuscular naltrexone because bleeding can occur at the IM injection site. All steps to avoid hematoma formation are recommended. Naltrexone extended-release injectable suspension (Vivitrol) is only for intramuscular administration; intravenous administration and subcutaneous administration should be avoided. The risk of serious injection site reactions may be increased when Vivitrol is deposited in subcutaneous or fatty tissue (see Adverse Reactions). Proper administration techniques and patient selection are imperative (see Administration). Consider alternate treatment for patients whose body habitus (obesity) precludes a gluteal intramuscular injection with the provided needle. Women may be physiologically at higher risk for injection site reactions because of typically higher gluteal fat thickness, and in fact, post-marketing reports of injection site reactions occur primarily in females. Also, a variable depth of subcutaneous tissue exists between patients; the depth is dependent on the gender and weight of the patient. Phentermine HCl Phentermine is contraindicated for use in any patient with a prior history of sympathomimetic amine hypersensitivity.[56][57] According to the manufactures of phentermine capsules and tablets, its products are contraindicated in patients with cardiac disease, advanced arteriosclerosis, moderate to severe hypertension, agitated states, or glaucoma.[58] Likewise, orally disintegrating tablets, are contraindicated in patients with a history of cardiac disease including coronary artery disease, stroke, cardiac arrhythmias, heart failure, and uncontrolled hypertension.[57] Valvular heart disease has been reported in women receiving the combination of fenfluramine and phentermine; the safety and efficacy of combination therapy with phentermine and any other drug products for weight loss, including selective serotonin reuptake inhibitors (e.g., fluoxetine, sertraline, fluvoxamine, paroxetine), have not been established. Therefore, coadministration of these drug products for weight loss is not recommended. Further, primary pulmonary hypertension (PPH) has been reported to occur in patients receiving a combination of phentermine with fenfluramine or dexfenfluramine. The possibility of an association between the use of phentermine alone and PPH or valvular heart disease cannot be ruled out. The initial symptom of PPH is usually dyspnea. Other initial symptoms include: angina pectoris, syncope, or lower extremity edema. Patients should be advised to report immediately any deterioration in exercise tolerance. Treatment should be discontinued in patients who develop new, unexplained symptoms of dyspnea, angina pectoris, syncope, or lower extremity edema. Because phentermine is a sympathomimetic agent, it is contraindicated in patients with hyperthyroidism. It should also be used with caution in patients with thyroid disease. Phentermine is contraindicated for use during or within 14 days following the use of MAOI therapy or other drugs with MAO-inhibiting activity. Monoamine oxidase inhibitors (MAOIs), or drugs that possess MAO-inhibiting activity such as furazolidone or procarbazine, can prolong and intensify the cardiac stimulation and vasopressor effects of phentermine.[56] Phentermine is contraindicated in patients with agitated states.aggravate these effects or cause an adverse drug reaction.[56] Symptoms of chronic intoxication include insomnia, irritability, change in personality, and psychotic symptoms that may be clinically indistinguishable from other psychotic disorders, like schizophrenia. Phentermine could aggravate certain mental conditions, such as those patients who exhibit highly nervous or agitated behavior, including psychosis, mania, or severe anxiety. The use of phentermine may cause dizziness, mask signs of fatigue or the need for rest, or impair the ability of a patient to participate in activities that require mental alertness. Advise patients to use caution when driving or operating machinery, or performing other tasks that require mental alertness until they are aware of how therapy will affect their mental and/or motor performance. In general, ethanol ingestion may aggravate these effects or cause an adverse drug reaction.[56] Advise patients to avoid alcohol while taking phentermine. Use phentermine cautiously in patients with diabetes mellitus. Insulin or other antidiabetic medication requirements may be altered in these patients when using phentermine during weight loss and due to altered dietary regimens. Patients should monitor their blood glucose regularly and follow the recommendations of their health care provider.[57] Appetite suppressant therapy is not recommend for use in those patients with a history of anorexia nervosa or other eating disorders. Use of phentermine is contraindicated in patients with a known history of drug or substance abuse. Phentermine is chemically and pharmacologically related to the amphetamines which have been extensively abused. The possibility of abuse of phentermine should be kept in mind when evaluating the desirability of including a drug as part of a weight reduction program. The least amount reasonable should be prescribed or dispensed at one time in order to limit the potential for overuse or drug diversion.[57] Phentermine products are now classified as FDA pregnancy risk category X, as are many anorexiants used for weight loss, and are contraindicated during pregnancy.[57][58] Safe use of phentermine during pregnancy has not been established; there is no known indication for use of phentermine during pregnancy. Phentermine should not be taken by pregnant women or by women who may become pregnant unless, in the opinion of the physician, the potential benefits outweigh the possible hazards.[58] Abrupt discontinuation of phentermine after prolonged high doses may result in severe mental depression or extreme fatigue; sleep EEG changes have also been noted. Gradual withdrawal of therapy is recommended. If immediate discontinuation is medically necessary, careful monitoring and symptom management is warranted.[56] Phentermine is contraindicated during breast-feeding.[57] It is not known whether phentermine and its metabolites are excreted in breast milk; however, because of the potential for serious adverse effects in the nursing infants, breast-feeding while taking phentermine is not recommended.[59][58] Safety and effectiveness of phentermine in children have not been established. Phentermine is not recommended for children or adolescents 16 years of age and under. There is no established use of phentermine in infants or neonates.[56][57] The debilitated or geriatric patient may be more susceptible to the CNS and sympathomimetic side effects of phentermine; use with caution in elderly patients. Patients with renal impairment may also be more susceptible to side effects. Exposure increases can be expected in patients with renal impairment or renal failure. Use caution when administering phentermine to patients with renal impairment.[56] The use of inhalational anesthetics during surgery may sensitize the myocardium to the effects of sympathomimetic drugs. Because of this, and its effects on blood pressure, in general, phentermine should be discontinued several days prior to surgery. Avoid abrupt discontinuation. Yohimbine HCl NOTE: Limited information about precautions and contraindications to yohimbine therapy exists. Yohimbine is contraindicated in patients with a hypersensitivity to yohimbine. Yohimbine should not be used in patients with a history of rauwolfia alkaloid hypersensitivity. Rauwolfia alkaloids include deserpidine, rauwolfia serpentina, or reserpine. Patients sensitive to these agents may also be sensitive to yohimbine. Yohimbine may worsen renal impairment, therefore administration of this drug in patients with renal disease or renal failure is contraindicated. Serious renal effects, including renal failure, have been reported to the FDA after the use of products containing yohimbe. Yohimbine should not be used concurrently with MAOI therapy (see Drug Interactions). Yohimbine should not be used in patients with angina pectoris, cardiac disease, or hypertension because these conditions may be aggravated or worsened by yohimbine. It is also recommended that this drug not be used in cardio-renal patients with history of peptic ulcer disease, children, and geriatric patients. Further, because yohimbine may enhance anxiety or other CNS symptoms, it should be used cautiously in patients with depression or other psychiatric illness. According to the German E Commission monographs, the use of yohimbine in those with hepatic disease is contraindicated. In theory, patients with hepatic impairment may exhibit impaired metabolism of yohimbine. Although recommendations on the use of yohimbine in those with hepatic disease are not available from the manufacturer, it should be noted that patients with hepatic disease have generally been excluded from participation in clinical trials that assess safety and efficacy of the drug. Therefore, it is advisable to avoid the use of yohimbine in those with hepatic disease, including biliary cirrhosis or hepatic failure. In general, yohimbine is not for use in females and must certainly not be used during pregnancy.[60] A FDA pregnancy risk category has not been assigned to this drug. However, given yohimbine's similarity to other rauwolfia alkaloids, it is suggested that yohimbine most closely corresponds to an FDA pregnancy risk category D (see Reserpine monograph). There is no known indication at this time for the use of yohimbine in pregnancy which would justify the potential risks to the fetus. Generally, this drug is not for use in females [60], and therefore should not be used during breast-feeding. Many of the rauwolfia alkaloids are excreted in human breast milk. A decision should be made to discontinue the medication or discontinue breast-feeding.
Caffeine
Caffeine has been noted to produce a variety of gastrointestinal (GI) effects. At therapeutic or nontoxic doses, caffeine can stimulate gastric secretions and may cause GI upset (dyspepsia), nausea, loose stools, and may aggravate gastroesophageal reflux disease (GERD).[39][36][38][64] Occasionally diarrhea is reported. The mild dehydration that caffeine produces may aggravate constipation. A temporary reduction in weight gain has also been reported. In a study comparing caffeine to placebo, the mean difference in weight gain was the greatest after 2 weeks of therapy.[65] Feeding intolerance (8.7%), gastritis (2.2%), and GI bleeding (2.2%) also occurred in the caffeine treatment groups.[36] During a controlled clinical trial of caffeine citrate in premature infants (n = 85 neonates), necrotizing enterocolitis was reported in 6 patients, 5 of whom were administered caffeine. Three of the infants died. The incidence was 4.3% in caffeine-treatment groups vs. 2.6% of placebo-treated infants. In a much larger clinical trial (n = 2,000 neonates) evaluating the use of caffeine citrate in apnea of prematurity, necrotizing enterocolitis was not more common in caffeine treated patients compared to placebo.[37][38][65] In a study evaluating the effect of caffeine on the splanchnic perfusion after a caffeine loading dose, the blood flow velocity was depressed for 2 to 3 hours after the infusion and slowly returned to baseline after approximately 6 hours.[66] Clinicians should be alert for signs and symptoms of gastric distress, abdominal bloating, nausea, vomiting, bloody stools, and lethargy in treated infants.[37][36] Excessive caffeine intake or intoxication in children, adolescents, and adults may cause vomiting along with other signs of caffeine intoxication.[64] In humans, a caffeine concentration of greater than 50 mg/L may produce toxic symptoms.
Caffeine is a CNS stimulant. Many adverse reactions to caffeine are an extension of caffeine’s pharmacologic actions. At therapeutic or nontoxic doses, caffeine can commonly cause nervousness, mild tremor, and heightened attentiveness.[64] Less frequent adverse reactions with usual consumption also include excitement, irritability, insomnia, headache, and muscle twitches.[67][68] Increased caffeine use among children and adolescents has been associated with insomnia, chronic headache, motor tics, irritability, learning difficulties, and other adverse health effects.[64][69][70] After excessive doses, caffeine can cause considerable anxiety. Seizures and delirium are also possible.[64] In humans, a caffeine level of > 50 mg/L may produce toxic symptoms. Other neurologic events have been reported in preterm neonates. In clinical trials of caffeine citrate in preterm neonates, cerebral hemorrhage (intracranial bleeding) was reported in 2.2% of treated patients versus 0% of neonates receiving placebo.[37]
Caffeine is a mild diuretic and patients may have increased urinary frequency. Polyuria can occur. Increased creatinine clearance and increased urinary calcium (hypercalciuria) and sodium excretion are reported in the literature.[37]
Adverse events to caffeine that have been described in the published literature include alterations in serum glucose such as hypoglycemia and hyperglycemia.[37]
In controlled clinical trials of caffeine citrate injection in premature neonates, the following adverse events occurred more commonly in caffeine-treatment groups than with placebo: accidental injury (2.2%), bleeding (2.2%), disseminated intravascular coagulation (2.2%), dyspnea (2.2%), pulmonary edema (2.2%), metabolic acidosis (2.2%), xerosis (2.2%), rash (unspecified) (8.7%), renal failure (unspecified) (2.2%), retinopathy of prematurity (2.2%), and skin breakdown (2.2%). In neonates, intolerance or overdose of caffeine may manifest as tachypnea. No deaths have been reported in relation to overdose of caffeine in neonates.[37]
Too much caffeine may occasionally cause rapid heartbeat.[71] Cardiovascular effects of caffeine have been reported in the literature (i.e., palpitations, sinus tachycardia, increased left ventricular output, and increased stroke volume).[37]
High caffeine intake has been reported to negatively affect sperm quality, including spermatogenesis inhibition). The propensity for caffeine to negatively affect fertility is controversial. Although controversial, infertility, as manifested by increased difficulty in getting pregnant, has been reported in females. Couples who are pursuing pregnancy should probably limit excessive intake of caffeine.
A distinct caffeine withdrawal syndrome has been described. Patients who consume or receive caffeine daily for several weeks experience notable physical and psychiatric responses including lethargy, anxiety, dizziness, or rebound headache upon caffeine withdrawal.[64]
DHEA
NOTE: Some prasterone, dehydroepiandrosterone, DHEA preparations are a combination of several hormones and/or herbs, and each individual component may need to be evaluated in the presence of adverse reactions. Only adverse reactions pertaining to DHEA are discussed in this monograph. Human side-effect data to date have been collected in non-systematic fashion via the FDA special nutritional adverse effect monitoring system (SNAEMS) or relatively small clinical trials.
DHEA has been observed to cause reversible reductions in HDL cholesterol and total cholesterol in some clinical trials; other trials have not noted changes in the serum lipid profile. DHEA may also exhibit anti-platelet effects. The influence of these changes on the development of side effects, atherosclerosis, or other cardiac-related endpoints is unknown.
In one 3-month study of 28 women with SLE, the following ADRs were noted in the females receiving DHEA: acneiform rash (57%), hirsutism (14%), weight gain (14%), menstrual irregularity (7%), and emotional lability (7%). The statistical significance of these side effects relative to placebo was not determined.[72] Some events commonly associated with SLE and reported as adverse events in clinical trials were less frequent in patients treated with prasterone (GL701) compared with placebo, including muscle pain, nasal and oral ulceration, and hair loss.
Prasterone, DHEA is a hormone with androgenic actions, however, the incidence of androgenic side effects is not known. When androgens are given to women, they may cause virilization, manifested by clitoromegaly, reduced breast size, and deepening of the voice or voice hoarseness. If treatment is discontinued when these symptoms first appear, they usually subside. Prolonged treatment with androgenic substances can lead to irreversible masculinity, so the benefit of DHEA treatment should be offset against the risk of androgen-like side effects.
The effect of prasterone or DHEA supplementation on normal endocrine processes in women is not clear. Women should report any menstrual changes, including amenorrhea, unusual vaginal bleeding, dysmenorrhea, or abdominal bloating to their health care providers. Breast changes, including breast discharge, breast enlargement, breast tenderness, or galactorrhea should also be reported.
Prasterone (DHEA) has androgenic actions, and it is not clear what effect prasterone may have in male patients. Similar to female patients, male patients may experience worsening of acne vulgaris. Male patients may theoretically experience feminization during prolonged therapy with DHEA resulting from inhibition of gonadotropin secretion and conversion of testosterone to estrogens. Feminizing effects in males might include gynecomastia. Feminizing effects secondary to androgens are generally reversible. It is not clear if DHEA would affect testicular function or prostatic function. Symptoms of urinary retention or urinary urgency, prostate pain, or signs of an enlarged prostate in a male patient should prompt clinical evaluation.
Mild peripheral edema can occur with DHEA use as the result of increased fluid retention (in association with sodium retention) and may be associated with mild weight gain.
Prasterone (DHEA) may cause emotional lability. At least one case of possible DHEA-induced mania has been reported in the literature, in a patient predisposed to bipolar illness who was consuming doses >= 300 mg/day PO on a routine basis. There was a temporal association between the time of drug use and the appearance of manic symptoms. Clinicians should be alert to possible alterations in psychiatric status in patients taking this medication for supplemental or medicinal purposes.
Hepatic dysfunction can occur from use of androgenic steroids, especially the oral 17-alpha-alkylandrogens (e.g., methyltestosterone). DHEA does not contain the 17-alkyl group in its structure, however, transient cases of drug-induced hepatitis in humans have been reported in association with DHEA use; these have included a few reports to the FDA Special Nutritionals Adverse Event Monitoring System (SN/AEMS). Liver toxicity has not been reported in human studies, but elevated hepatic transaminases have been reported and confirmed upon rechallenge in some trials. In 1984, the FDA banned the non-prescription (OTC) sale of DHEA due to concern over hepatitis. Clastogenesis has been noted in hepatic tissues of animals exposed to DHEA. DHEA appears to act as a perisoxome proliferator, resulting in liver tumors and nodules in the periportal areas of the liver lobule in rats. DHEA should be discontinued in any patient developing signs or symptoms of potential liver problems, including elevated hepatic enzymes, continued nausea and vomiting, fatigue, jaundice, or severe abdominal pain; the patient should be evaluated.
In studies of male patients with HIV virus infection, side effects attributed to DHEA treatments and confirmed upon rechallenge included nasal congestion, fatigue, headache, and mild insomnia.[2]
Prasterone (DHEA) therapy is reported to cause libido increase. No objective evidence of this side effect exists at this time.
The effect of DHEA on the progression of hormonally-dependent tumors in males or females, or the risk of secondary malignancy, such as breast cancer, is not known. One case-control study of women with ovarian cancer demonstrated higher serum androstenedione and DHEA/DHEAS levels in patients with ovarian tumors versus controls.[73] Whether DHEA supplementation would be associated with similar the serum hormonal profiles is unknown. Male breast cancer, prostate cancer and prostatic hypertrophy can develop due to endocrine epithelial cell growth during therapy with androgens. One case report has been published of a patient with advanced prostate cancer who was symptomatically treated with DHEA. The patient experienced a “flare” of his cancer during the treatment period.[74] A causal relationship has not been established. Widespread use of DHEA supplements in men or women should be discouraged until more is known about potential secondary malignancy risks.
Prasterone, dehydroepiandrosterone (DHEA) is an androgenic hormone and may potentially cause teratogenesis or changes the ability to conceive or carry a viable pregnancy. Dehydroepiandrosterone, DHEA should be considered contraindicated in pregnancy, similar to other androgenic hormones. It is assumed that exogenous DHEA supplementation to a pregnant woman could potentially have deleterious effects on fetal development or viability. No controlled trials of DHEA in primate or human gestation exist. If pregnancy is suspected, pregnancy should be ruled out before continuing DHEA use.
Methionine
Adverse reactions reported following methionine administration include gastrointestinal disorder: Nausea and vomiting and drowsiness [75]
Methylcobalamin
In most cases, methylcobalamin is nontoxic, even in large doses. Adverse reactions reported following methylcobalamin administration include headache, infection, nausea/vomiting, paresthesias, and rhinitis. Adverse reactions following intramuscular (IM) injection have included anxiety, mild transient diarrhea, ataxia, nervousness, pruritus, transitory exanthema, and a feeling of swelling of the entire body. Some patients have also experienced a hypersensitivity reaction following intramuscular injection that has resulted in anaphylactic shock and death. In cases of suspected cobalt hypersensitivity, an intradermal test dose should be administered.
During the initial treatment period with methylcobalamin, pulmonary edema and congestive heart failure have reportedly occurred early in treatment with parenteral methylcobalamin. This is believed to result from the increased blood volume induced by methylcobalamin. Peripheral vascular thrombosis has also occurred. In post-marketing experience, angioedema and angioedema-like reactions were reported with parenteral methylcobalamin.
Hypokalemia and thrombocytosis could occur upon conversion of severe megaloblastic anemia to normal erythropoiesis with methylcobalamin therapy. Therefore, monitoring of the platelet count and serum potassium concentrations are recommended during therapy. Polycythemia vera has also been reported with parenteral methylcobalamin.
Diarrhea and headache.
Call your health care provider immediately if you are experiencing any signs of an allergic reaction: skin rash, itching or hives, swelling of the face, lips, or tongue, blue tint to skin, chest tightness, pain, difficulty breathing, wheezing, dizziness, red, swollen painful area on the leg.
Naltrexone HCl
Naltrexone can cause hepatocellular injury when given in excessive doses. Naltrexone does not appear to be a hepatotoxin at the recommended doses. The hepatotoxic potential of naltrexone has been described in a placebo-controlled study using a 300 mg/day dose of naltrexone. In this study, 20% of patients experienced elevated hepatic enzymes (3—19 times baseline values). All patients were asymptomatic, and transaminase levels returned to baseline or decreased in a matter of weeks. Other studies of naltrexone doses > 50 mg/day in patients with opiate dependence or alcoholism also resulted in increased hepatic enzymes. Clinical trial data indicate that 7—13% of study patients receiving 380 mg of intramuscular naltrexone experienced elevated hepatic enzymes compared to 2—6% of those on placebo.[76] Hepatitis, elevated hepatic enzymes, and hyperbilirubinemia have been reported in post-marketing reports with naltrexone. Warn patients of the risk of hepatic injury, and advise them to get immediate medical attention if they experience symptoms of acute hepatitis. A high index of suspicion for drug-related hepatic injury is critical if the occurrence of naltrexone-induced liver damage is to be detected at the earliest possible time. Evaluations to detect liver injury are recommended at a frequency appropriate to the clinical situation and to the naltrexone dose. Discontinue naltrexone if symptoms or signs of acute hepatitis develop.[52]
Central nervous system (CNS) effects occurring during clinical trials of oral naltrexone for alcohol or opiate dependence included headache (>= 7%), dizziness (4—9%), nervousness (>= 4%), insomnia (>= 3%), anxiety (>= 2%), fatigue (>= 4%), drowsiness (<= 2%), increased energy (< 10%), irritability (< 10%), paranoia (< 1%), restlessness (< 1%), confusion (< 1%), disorientation (< 1%), hallucinations (< 1%), nightmares (< 1%), yawning (< 1%), and hot flashes (< 1%).[52] During clinical trials using 380 mg of extended-release injectable naltrexone suspension for alcohol opioid dependence, the following effects were reported more frequently with the active drug than placebo: dizziness or syncope (13% vs 4%), insomnia (6—14% vs 1—12%), headache (3—25% vs 2—18%), drowsiness (4% vs 1%), and anxiety (12% vs 8%).[76] Cerebral arterial aneurysm, seizures, mental impairment, dysgeusia, euphoric mood (euphoria), migraine, ischemic stroke, irritability, disturbance in attention, abnormal dreams, agitation, delirium, hot flashes, and paresthesias were also reported during clinical trials of intramuscular naltrexone; however, the incidence of these effects is not known. CNS effects reported during post-marketing use of naltrexone include abnormal thinking, agitation, anxiety, headache, fatigue, confusion, euphoria, hallucinations, insomnia, nervousness, drowsiness, hot flashes, dizziness, and hyperkinesis. It is not always possible to distinguish these occurrences from signs and symptoms of naltrexone-induced opiate discontinuation syndrome.[52] Depression, suicidal ideation, and attempted suicide have been reported in individuals receiving oral naltrexone, placebo, and in concurrent control groups undergoing treatment for alcoholism and opiate dependence.[52] In controlled clinical trials of the extended-release injectable suspension of naltrexone, suicidal ideation, suicide attempts, or completed suicides occurred in 1% of patients and in no patients treated with placebo. In some cases, the suicidal thoughts or behavior occurred after study discontinuation but were in the context of an episode of depression that began while the patient was taking naltrexone. Two completed suicides occurred in patients who were taking naltrexone. Depression-related events associated with premature discontinuation of naltrexone also occurred in about 1% of patients and in no patients treated with placebo. In the 24-week, placebo-controlled, pivotal trial, adverse events involving depressed mood were reported by 10% of patients treated with naltrexone 380 mg IM as compared with 5% of patients treated with placebo. Monitor patients for the development of depression or suicidal thinking. Families and caregivers of patients being treated with naltrexone should be alerted to the need to monitor patients for the emergence of symptoms of depression or suicidality and to report such symptoms to the patient's health care provider. Physicians should be aware that treatment with naltrexone does not reduce the risk of suicide in patients.[76] In clinical trials of the extended-release injectable suspension of naltrexone, patients who took naltrexone had increases in eosinophil counts (eosinophilia) relative to patients on placebo, but eosinophil counts returned to normal over a period of several months in the patients who continued to take naltrexone. One diagnosed case and 1 suspected case of eosinophilic pneumonia occurred. The pneumonia resolved with antibiotics and corticosteroids. Consider eosinophilic pneumonia if progressive shortness of breath and hypoxia develop and if patients do not respond to antibiotics.[76] Patients treated with naltrexone 380 mg IM experienced a mean maximal decrease in platelet count of 17,800/mm3 as compared with 2600/mm3 in placebo patients. In randomized controlled trials, naltrexone administration was not associated with an increase in bleeding related adverse events. Idiopathic thrombocytopenic purpura was reported in one patient who may have been sensitized to naltrexone in a previous course of treatment with naltrexone. The condition cleared without sequelae after discontinuation of naltrexone and corticosteroid treatment. In addition, deep vein thrombosis and pulmonary embolism were reported as treatment-emergent adverse reactions during clinical trials of naltrexone suspension for injection; the incidences are unknown.[76] Gastrointestinal (GI) effects occurring during clinical trials of oral naltrexone for alcohol or opiate dependence include nausea (>= 10%), vomiting (>= 3%), abdominal pain (> 10%), anorexia (< 10%), diarrhea (< 10%), constipation (< 10%), appetite stimulation (< 1%), weight loss (< 1%), weight gain (< 1%), xerostomia (< 1%), flatulence (< 1%), hemorrhoids (< 1%), and peptic ulcer (< 1%).[52] During controlled trials of oral naltrexone 50 mg/day in alcohol dependence, approximately 5% of patients discontinued naltrexone due to nausea. During clinical trials using 380 mg of extended-release injectable naltrexone suspension for alcohol or opioid dependence, the following GI effects were reported more frequently with 380 mg of the active drug than placebo: nausea (33% vs 11%), vomiting (14% vs 6%), diarrhea (13% vs 10%), abdominal pain (11% vs 8%), xerostomia (5% vs 4%), dental pain (toothache 4% vs 2%), and anorexia (14% vs 3%).[76] Weight loss, weight gain, abdominal discomfort, colitis, constipation, flatulence, appetite stimulation, gastroenteritis, gastroesophageal reflux disease (GERD), GI bleeding, hemorrhoids, acute pancreatitis, paralytic ileus, and perirectal abscess were also reported. In post-market experience of oral naltrexone, GI effects including anorexia, nausea, vomiting, abdominal pain, and diarrhea have been reported. It is not always possible to distinguish these occurrences from signs and symptoms of naltrexone-induced opiate discontinuation syndrome.[52] Injection site reactions have been precipitated following self-administration of the naltrexone extended-release suspension (e.g., Vivitrol). Inform patients that the injection must be prepared by and administered by a healthcare professional. Of 440 patients who received 380 mg of the extended-release injectable suspension of naltrexone (Vivitrol) in clinical trials for alcohol dependence, 69% had an injection site reaction (pain, tenderness, induration, swelling, or itching) versus 50% of those receiving a placebo injection. Specific injection site reactions that occurred more frequently in the active treatment group than the placebo group included injection site tenderness (45% vs 39%), injection site induration (35% vs. 8%), injection site pain (5% to 17% vs. 1% to 7%), nodules/swelling (15% vs. 4%), itching at the injection site (10% vs. 0%), and injection site ecchymosis (7% vs. 5%). One patient developed an area of induration at the injection site that continued to enlarge after 4 weeks. Eventually, necrotic tissue that required surgical excision developed. The FDA has received 196 reports of injection site reactions including cellulitis, induration, hematoma, abscess, sterile abscess, and tissue necrosis. Sixteen patients required surgical intervention ranging from incision and drainage in the cases of abscesses to extensive surgical debridement in the cases that resulted in tissue necrosis. The extended-release injectable suspension of naltrexone should only be administered intramuscularly (IM); the risk of serious injection site reactions may be increased when Vivitrol is deposited in subcutaneous or fatty tissue. Instruct patients to monitor the injection site and to get medical care if they develop pain, swelling, tenderness, induration, bruising, itching, or redness at the injection site that does not improve or worsens within 2 weeks. Promptly refer patients with worsening injection site reactions to a surgeon.[76] Urticaria, angioedema, and anaphylactoid reactions (anaphylaxis) have occurred in association with naltrexone administration in both clinical trials and during post-marketing use. Patients should be advised of the potential for serious hypersensitivity reactions while using naltrexone and instructed to seek immediate medical attention in the event of such a reaction.[76] During clinical trials using 380 mg of intramuscular (IM) naltrexone, infections reported more frequently within the active drug group than the placebo group included nasopharyngitis (7% vs 2%) and influenza (5% vs 4%).[76] Other respiratory or related effects that were reported during IM naltrexone clinical trials included upper respiratory tract infection, advanced HIV disease in HIV-infected patients, bronchitis, chronic obstructive pulmonary disease, dyspnea, laryngitis, pharyngolaryngeal pain, pneumonia, sinus congestion, and sinusitis. Respiratory effects or symptoms of infection occurring in less than 1% of patients during clinical trials of oral naltrexone for opiate dependence included nasal congestion, rhinorrhea, sneezing, sore throat, excess mucus, sinus trouble, hoarseness, cough, fever, and dyspnea.[52] Additionally, eosinophilic pneumonia, which may present as dyspnea, coughing, and/or hypoxia, has been reported in association with injectable naltrexone use (see eosinophilic pneumonia). In clinical trials of intramuscular naltrexone (380 mg) in patients with opioid dependence, 5% of study patients experienced hypertension compared to 3% of those on placebo.[76] Other cardiovascular effects observed during clinical trials of intramuscular naltrexone included angina, atrial fibrillation, congestive heart failure, coronary artery atherosclerosis, myocardial infarction, and palpitations. Cardiovascular effects occurring in less than 1% of patients during clinical trials of oral naltrexone for opiate dependence included epistaxis, phlebitis, edema, increased blood pressure, unspecified ECG changes, palpitations, and sinus tachycardia. Cardiac effects reported during post-marketing use of naltrexone include chest pain (unspecified), palpitations, and changes in blood pressure. It is not always possible to distinguish these occurrences from signs and symptoms of naltrexone-induced opiate discontinuation syndrome.[52] During clinical trials using 380 mg of intramuscular naltrexone suspension for opioid dependence, the following musculoskeletal effects or pain symptoms were reported more frequently with the active drug than placebo: arthralgia (12% vs 5%), back pain (6% vs 5%), and muscle cramps (8% vs 1%).[76] Myalgia, joint stiffness, limb pain, and muscle spasms have also been reported. Musculoskeletal effects or pain symptoms occurring during clinical trials of oral naltrexone for opiate dependence included arthralgia and myalgia (> 10%), shoulder pain (< 1%), knee or leg pain (< 1%), tremor (< 1%), twitching (< 1%), inguinal pain (< 1%), and side pain.[52] Tremor and myalgia have been reported during post-marketing use of naltrexone. It is not always possible to distinguish these occurrences from signs and symptoms of naltrexone-induced opiate discontinuation syndrome. Increased creatinine phosphokinase (CPK) concentrations have been associated with naltrexone use. In open-label trials, 16% of patients dosed for more than 6 months had increases in CPK. Increases in 1—2 times the upper limit of normal (ULN) were most common for both the oral naltrexone and IM naltrexone 380 mg groups. Although CPK elevations of 1—2 times ULN were most commonly encountered, elevations as high as 4 times ULN for the oral naltrexone group and 35 times ULN for the IM naltrexone group were noted. However, there were no differences between the placebo and either the oral or IM naltrexone groups with respect to the proportions of patients with a CPK value at least 3 times ULN. No factors other than naltrexone exposure were associated with the CPK elevations.[52] Dermatologic or related effects occurring during clinical trials of oral naltrexone for opiate dependence included rash (unspecified) (< 10%), oily skin (< 1%), pruritus (< 1 %), acne vulgaris (< 1%), tinea pedis (< 1%), cold sores (< 1%), and alopecia (< 1%).[52] During clinical trials using 380 mg of intramuscular naltrexone suspension, rash occurred more frequently with active drug than placebo (6% vs 4%).[76] Other related effects reported with the intramuscular formulation included night sweats, pruritus, heat exhaustion, and hyperhidrosis. Rash and increased sweating have also been reported during post-marketing use of naltrexone. It is not always possible to distinguish these occurrences from signs and symptoms of naltrexone-induced opiate discontinuation syndrome.[52] Genitourinary (GU) effects occurring during clinical trials of oral naltrexone included ejaculation dysfunction (delayed ejaculation < 10%), dysuria (< 1%), increased urinary frequency (< 1%), and libido increase or libido decrease (< 1%).[52] Decreased libido and urinary tract infection have been reported with the use of the intramuscular formulation.[76] Special senses effects (otic, ophthalmic) occurring in less than 1% of patients during clinical trials of oral naltrexone included blurred vision, ocular irritation (burning), light sensitivity (photophobia), eye swelling/ache (ocular inflammation), otalgia, and tinnitus. Unspecified visual impairment has been reported during post-marketing use of oral naltrexone.[52] Conjunctivitis and blurred vision have also been reported with the use of the intramuscular formulation. Retinal artery occlusion has been reported rarely after injection with another drug product containing polylactide-co-glycolide (PLG) microspheres. This event has been reported in the presence of abnormal arteriovenous anastomosis. No cases of retinal artery occlusion have been reported during clinical trials or post-market use of the intramuscular formulation of naltrexone.[76] Lymphadenopathy and increased white blood cell count have been reported with the use of naltrexone extended-release suspension for injection during clinical trials.[76] Acute cholecystitis and cholelithiasis have been reported as treatment-emergent adverse effects in patients who received naltrexone extended-release suspension for injection for alcohol and/or opioid dependence; the incidence of these effects is unknown.[76] General effects occurring during clinical trials of oral naltrexone for opiate dependence included increased thirst (polydipsia) (< 10%), chills (< 10%), swollen glands (< 1%), and cold feet (< 1%).[52] During clinical trials using 380 mg of intramuscular naltrexone suspension for opioid dependence, asthenia was reported more frequently in the active treatment group than the placebo group (23% vs 12%). Other general events observed during clinical trial evaluation of intramuscular naltrexone included chest tightness, chills, face edema, pyrexia, rigors, and lethargy. Malaise and asthenia have been reported during post-market use of oral naltrexone.[76] During clinical trial evaluation of intramuscular naltrexone suspension, metabolic or nutritional effects including dehydration and hypercholesterolemia were observed; however, the frequencies are unknown. In some individuals, the use of opiate antagonists has been associated with a change in baseline levels of some hypothalamic, pituitary, adrenal, or gonadal hormones. The clinical significance of these changes is not fully understood.[76] Abrupt withdrawal precipitated by administration of an opioid antagonist to an opioid-dependent patient may result in a withdrawal syndrome severe enough to require hospitalization, and in some cases management in the intensive care unit. Opioid withdrawal has been precipitated following self-administration of the naltrexone extended-release suspension (e.g., Vivitrol). Inform patients that the injection must be prepared by and administered by a healthcare professional. To prevent precipitation of withdrawal, patients should be opioid-free for a minimum of 7 to 10 days prior to initiation of naltrexone. When transitioning from buprenorphine or methadone, patients may be vulnerable to precipitation of withdrawal symptoms for up to two weeks. Precipitated opioid withdrawal has also been observed in alcohol-dependent patients in circumstances where the prescriber had been unaware of the additional use of opioids or co-dependence on opioids. Make patients aware of the risks associated with precipitated withdrawal and the need to give an accurate account of last opioid use. Studies of naltrexone in alcoholic populations and in volunteers in clinical pharmacology studies have suggested that a small fraction of patients may experience an opioid discontinuation-like symptom complex including, but not limited to, tearfulness, abdominal cramps, bone, muscle, or joint pain, nasal symptoms, and feeling restless. These symptoms may represent the unmasking of occult opioid use or it may represent symptoms attributable to naltrexone. Patients treated for alcohol dependence with naltrexone should be assessed for underlying opioid dependence and for any recent use of opioids prior to initiation of treatment. Because there is no completely reliable method for determining whether a patient has had an adequate opioid-free period, prescribers should always be prepared to manage withdrawal symptomatically with non-opioid medications. A naloxone challenge test may be helpful; however, a few case reports have indicated that patients may experience precipitated withdrawal despite having a negative urine toxicology screen or tolerating a naloxone challenge test (usually in the setting of transitioning from buprenorphine treatment). Withdrawal symptoms and death have been reported during the use of naltrexone in ultra rapid detoxification programs; the causes of death are not known. If rapid transition from agonist to antagonist therapy is considered necessary and appropriate by the healthcare provider, patients should be closely monitored in an appropriate medical setting where precipitated withdrawal can be managed.[76][52] Phentermine HCl Central nervous system adverse reactions that have been reported in patients receiving phentermine include dizziness, dysphoria, euphoria, headache, insomnia, overstimulation, restlessness, and tremor. Psychosis at recommended doses may occur rarely in some patients.[34][77][78][79] Primary pulmonary hypertension (PPH) and cardiac valvulopathy (regurgitant cardiac valvular disease) have been reported with phentermine. The initial symptom of PPH is usually dyspnea; other initial symptoms include: angina pectoris, syncope, or peripheral edema. Patients should be advised to report immediately any deterioration in exercise tolerance. Treatment should be discontinued in patients who develop new, unexplained symptoms of dyspnea, angina pectoris, syncope, or peripheral edema. Other cardiovascular adverse effects that have been reported include hypertension, ischemic events, palpitations, and sinus tachycardia.[34][77][78][79] Reported adverse gastrointestinal effects of phentermine include constipation, diarrhea, dysgeusia, nausea, and xerostomia.[34][77][78][79] Impotence (erectile dysfunction), libido increase, and libido decrease have been reported in patients receiving phentermine.[34][77][78][79] Urticaria has been reported in patients receiving phentermine.[34][77][78][79] Phentermine has not been systematically studied for its potential to produce dependence in obese patients treated with usual recommended dose ranges. Phentermine is related chemically and pharmacologically to the amphetamines, and these stimulant drugs have been extensively abused and the possibility of abuse of phentermine should be kept in mind when evaluating the desirability of including this drug product as part of a weight reduction program. Abuse of amphetamines and related drugs (e.g., phentermine) may be associated with intense psychological dependence and severe social dysfunction.[78][34][77][79] There are reports of patients who have increased the dosage of these drugs to many times than recommended. Physical dependence (physiological dependence) is a state that develops as a result of physiological adaptation in response to repeated drug use. Physical dependence manifests by drug-class-specific withdrawal symptoms after abrupt discontinuation or a significant dose reduction of a drug. Limited data are available for phentermine. Abrupt cessation following prolonged high dosage administration results in extreme fatigue and mental depression; changes are also noted on a sleep electroencephalogram. Thus, in situations where rapid withdrawal is required, appropriate medical monitoring is recommended.[78][34][77][79] Evidence-based data from the literature are relatively limited, and some experts suggest that long-term phentermine pharmacotherapy for obesity does not induce abuse or psychological dependence (addiction), drug craving, and that abrupt treatment cessation within the normal prescription dose range does not induce amphetamine-like withdrawal.[80] More data are needed to confirm the dependence potential of phentermine-containing obesity products. Tolerance to the anorexiant effects of phentermine usually develops within a few weeks of starting therapy. The mechanism of tolerance appears to be pharmacodynamic in nature; higher doses of phentermine are required to produce the same response. When tolerance develops to the anorexiant effects, it is generally recommended that phentermine be discontinued rather than the dose increased. The maximum recommended dose should not be exceeded.[34][77][78][79] Yohimbine HCl Yohimbine readily crosses the blood-brain barrier and can therefore produce central nervous system adverse reactions. The most common CNS adverse reactions include anxiety, antidiuresis, dizziness, flushing, headache, hypertension, increased motor activity, irritability, nervousness or restlessness, sinus tachycardia, and tremor. Although yohimbine is not administered intravenously, diaphoresis, nausea and vomiting have been reported following IV administration of yohimbine. Per the FDA (1993 out of print document), natural Yohimbe is a tree bark containing a variety of pharmacologically active chemicals; the major identified alkaloid in yohimbe is yohimbine. Yohimbe is marketed in a number of dietary supplements for body building and 'enhanced male performance.' Serious adverse effects, including renal failure (unspecified), seizures and death, have been reported to FDA with products containing yohimbe. Side effects that are well recognized may include central nervous system stimulation that causes anxiety attacks or agitation. At high doses, yohimbine is reported to inhibit monoamine oxidase (MAO). MAO inhibitors (MAOIs) can cause serious adverse effects (like severe hypertension) when taken concomitantly with tyramine-containing foods (e.g., liver, cheeses, red wine) or with over-the-counter (OTC) products containing phenylpropanolamine (PPA). Patients taking yohimbe should be warned to avoid these foods and PPA because of the increased likelihood of adverse effects.
Caffeine
Caffeine citrate is used for neonatal apnea so concerns for teratogenicity are not relevant when administered to infants, however, when 50 mg/kg of sustained-release pellets were administered to pregnant mice during the period of organogenesis, a low incidence of cleft palate and exencephaly have been noted in the fetuses.[37] Caffeine easily crosses the placenta; fetal blood and tissue concentrations approximate maternal concentrations. There are no large, well-controlled studies of caffeine administration in pregnant women; it is generally recommended that the intake of caffeine-containing beverages, like coffee, teas, and sodas, be limited in pregnancy (usually no more than 1 to 2 caffeine-containing beverages/day) or avoided if possible. Caffeine-containing medications should likewise, be limited to use only when absolutely necessary. Low to moderate caffeine intake does not appear to increase the risk of congenital malformation, spontaneous abortion, pre-term birth or low birth weight. The association between high daily intake (more than 500 mg/day) of caffeine and increased rates of low birth weight, spontaneous abortion, difficulty in getting pregnant or infertility is still controversial, as some studies have not controlled for concomitant cigarette smoking.[40] There are no adequate and well-controlled studies of caffeine administration in pregnant women. Neonatal arrhythmias (e.g., tachycardia, premature atrial contractions) and tachypnea have been reported when caffeine was consumed during pregnancy in amounts > 500 mg/day; caffeine withdrawal after birth may account for these symptoms.[41]Caffeine citrate is used for neonatal apnea so concerns for teratogenicity are not relevant when administered to infants, however, when 50 mg/kg of sustained-release pellets were administered to pregnant mice during the period of organogenesis, a low incidence of cleft palate and exencephaly have been noted in the fetuses.[37] Caffeine easily crosses the placenta; fetal blood and tissue concentrations approximate maternal concentrations. There are no large, well-controlled studies of caffeine administration in pregnant women; it is generally recommended that the intake of caffeine-containing beverages, like coffee, teas, and sodas, be limited in pregnancy (usually no more than 1 to 2 caffeine-containing beverages/day) or avoided if possible. Caffeine-containing medications should likewise, be limited to use only when absolutely necessary. Low to moderate caffeine intake does not appear to increase the risk of congenital malformation, spontaneous abortion, pre-term birth or low birth weight. The association between high daily intake (more than 500 mg/day) of caffeine and increased rates of low birth weight, spontaneous abortion, difficulty in getting pregnant or infertility is still controversial, as some studies have not controlled for concomitant cigarette smoking.[40] There are no adequate and well-controlled studies of caffeine administration in pregnant women. Neonatal arrhythmias (e.g., tachycardia, premature atrial contractions) and tachypnea have been reported when caffeine was consumed during pregnancy in amounts > 500 mg/day; caffeine withdrawal after birth may account for these symptoms.[41]
DHEA
DHEA should be considered a pregnancy category X drug, similar to other androgenic hormones. Studies of the role of endogenous fetal and maternal DHEA in pregnancy indicate that the ratio of DHEA or DHEAS to other hormones in the serum or placenta may influence the processes of fetal development, parturition, and labor. Endogenous DHEA and DHEAS appear to be important in the functional development of the adrenal cortex and other endocrine activities in the fetus; it is assumed that exogenous DHEA supplementation to a pregnant woman could potentially have deleterious effects on fetal development or viability. The androgenic effects of DHEA could potentially result in masculinization of a female fetus. No controlled trials of DHEA in primate or human gestation exist. Do not administer DHEA to a pregnant woman.
Inositol
Given its use in the treatment of polycystic ovarian syndrome and gestational diabetes, myo-inositol may be considered relatively safe during pregnancy. In a meta-analysis of randomized controlled trials, 2 g of myo-inositol administered orally twice daily was reported to be safe during pregnancy.[61] However, high concentrations of D-chiro-inositol negatively affect the quality of oocytes.[62] Therefore, D-chiro-inositol may not be used by women seeking to get pregnant. Effects of other inositol isomers are not well characterized.
Methionine
Excess methionine in the maternal diet may be detrimental to fetal development. This is because additional glycine and serine may be required to catabolize the excess methionine, inadvertently resulting in the deficiency of these amino acids. Excess methionine may also be metabolized to homocysteine. Elevated plasma homocysteine levels are associated with preeclampsia, spontaneous abortion, placental rupture, and miscarriage.[63]
Methylcobalamin
Parenteral methylcobalamin is classified as pregnancy category C. Adequate studies in humans have not been conducted; however, no maternal or fetal complications have been associated with doses that are recommended during pregnancy, and appropriate treatment should not be withheld from pregnant women with vitamin B12 responsive anemias. Conversely, pernicious anemia resulting from vitamin B12 deficiency may cause infertility or poor pregnancy outcomes. Vitamin B12 deficiency has occurred in breast-fed infants of vegetarian mothers whose diets contain no animal products (e.g., eggs, dairy), even though the mothers had no symptoms of deficiency at the time. Maternal requirements for vitamin B12 increase during pregnancy. The usual daily recommended amounts of methylcobalamin, vitamin B12 either through dietary intake or supplementation should be taken during pregnancy (see Dosage).
Naltrexone HCl
Naltrexone is classified as FDA pregnancy risk category C. There are no adequate and well-controlled studies in pregnant women. In some individuals, opiate antagonists have been associated with a change in baseline levels of some hypothalamic, pituitary, adrenal, or gonadal hormones, although the clinical significance is not known. In rat studies, there was an increase in early fetal loss and pseudopregnancy, and a decrease in pregnancy rate. There was no evidence of teratogenicity; however, rats do not form a significant amount of the major human metabolite, 6-B-naltrexol; therefore, the potential reproductive toxicity of 6-B-naltrexol in rats is not known. There were small increases in the numbers of testicular mesotheliomas in male rats and vascular tumors in female rats during a 2-year carcinogenicity study; however, no evidence of carcinogenicity was observed in mice.[52] When considering the use of naltrexone during pregnancy for relapse prevention in alcohol or opiate dependence, the risks to the fetus of continued substance abuse by the mother should be weighed against the potential adverse effects from fetal exposure to naltrexone. Drug therapy should be considered only if supportive substance abuse prevention measures are ineffective. The effects of naltrexone during labor and delivery are unknown.
Phentermine HCl
Phentermine products are now classified as FDA pregnancy risk category X, as are many anorexiants used for weight loss, and are contraindicated during pregnancy.[57][57] Safe use of phentermine during pregnancy has not been established; there is no known indication for use of phentermine during pregnancy. Phentermine should not be taken by pregnant women or by women who may become pregnant unless, in the opinion of the physician, the potential benefits outweigh the possible hazards.[57]
Yohimbine HCl
In general, yohimbine is not for use in females and must certainly not be used during pregnancy.[60] A FDA pregnancy risk category has not been assigned to this drug. However, given yohimbine’s similarity to other rauwolfia alkaloids, it is suggested that yohimbine most closely corresponds to an FDA pregnancy risk category D (see Reserpine monograph). There is no known indication at this time for the use of yohimbine in pregnancy which would justify the potential risks to the fetus.
Caffeine
Although the American Academy of Pediatrics has considered the use of mild to moderate use of caffeinated beverages to be compatible with lactation, mothers who are breast-feeding should limit their intake of caffeinated beverages if possible.[42] Caffeine-containing drug-products should be used cautiously during lactation due to their high caffeine contents. Mothers who are breast-feeding infants who have been prescribed caffeine for apnea should generally avoid additional caffeine use.[37] The CYPP450 hepatic metabolism of caffeine is inhibited in infants who are breastfed; formula feeding does not appear to affect the pharmacokinetics of caffeine in infants.[43] Peak caffeine milk levels usually occur within 1 hour after the maternal ingestion of a caffeinated beverage; with milk: plasma ratios of 0.5 to 0.7 reported.[44][45] Although only small amounts are secreted in breast milk, caffeine can accumulate in the neonate if maternal ingestion is moderate to high. Higher caffeine intake (more than 500 mg/day) by a nursing mother may cause irritability or poor sleeping patterns in the infant who is breast-feeding.[46] Consider the benefits of breast-feeding, the risk of potential infant drug exposure, and the risk of an untreated or inadequately treated condition.
DHEA
DHEA is a hormone and should not be supplemented in a lactating woman who is breast-feeding her infant. Most hormones are excreted in breast milk. Like other androgenic hormones, it is possible that DHEA could inhibit lactation. It is unknown what effect DHEA would have on the breast-feeding infant.
Inositol
Given its use in the treatment of polycystic ovarian syndrome and gestational diabetes, myo-inositol may be considered relatively safe during pregnancy. In a meta-analysis of randomized controlled trials, 2 g of myo-inositol administered orally twice daily was reported to be safe during pregnancy.[61] However, high concentrations of D-chiro-inositol negatively affect the quality of oocytes.[62] Therefore, D-chiro-inositol may not be used by women seeking to get pregnant. Effects of other inositol isomers are not well characterized.
Methionine
Excess methionine in the maternal diet may be detrimental to fetal development. This is because additional glycine and serine may be required to catabolize the excess methionine, inadvertently resulting in the deficiency of these amino acids. Excess methionine may also be metabolized to homocysteine. Elevated plasma homocysteine levels are associated with preeclampsia, spontaneous abortion, placental rupture, and miscarriage.[63]
Methylcobalamin
Methylcobalamin is distributed into breast milk in amounts similar to those in maternal plasma, and distribution in breast milk allows for adequate intakes of methylcobalamin by breast-feeding infants. Adequate maternal intake is important for both the mother and infant during nursing, and maternal requirements for vitamin B12 increase during lactation. According to the manufacturer, the usual daily recommended amounts of methylcobalamin, vitamin B12 for lactating women should be taken maternally during breast-feeding (see Dosage). The American Academy of Pediatrics considers vitamin B12 to be compatible with breast-feeding. Consider the benefits of breast-feeding, the risk of potential infant drug exposure, and the risk of an untreated or inadequately treated condition. If a breast-feeding infant experiences an adverse effect related to a maternally ingested drug, healthcare providers are encouraged to report the adverse effect to the FDA.
Naltrexone HCl
According to the manufacturer, naltrexone and its metabolite are excreted into human milk, and a decision should be made to discontinue breastfeeding or discontinue naltrexone, taking into consideration the importance of the drug to the mother. Animal studies have shown the potential for tumorigenicity.[52] No reports describing the use of naltrexone during breastfeeding are available. According to the American Academy of Pediatrics (AAP), the maternal ingestion of large amounts of ethanol or opiates can cause adverse effects in the nursing infant.[55] If supportive substance abuse prevention measures are ineffective, the risks to the nursing infant of continued ethanol or opiate abuse by the mother should be weighed against the potential for adverse drugs effects when determining whether to use naltrexone as a substance abuse-deterrent during breast-feeding.
Phentermine HCl
Phentermine is contraindicated during breastfeeding.[57] It is not known whether phentermine and its metabolites are excreted in breast milk; however, because of the potential for serious adverse effects in the nursing infants, breast-feeding while taking phentermine is not recommended.[59][58]
Yohimbine HCl
Generally, this drug is not for use in females [60], and therefore should not be used during breastfeeding. Many of the rauwolfia alkaloids are excreted in human breast milk. A decision should be made to discontinue the medication or discontinue breastfeeding.
Store this medication at 68°F to 77°F (20°C to 25°C) and away from heat, moisture and light. Keep all medicine out of the reach of children. Throw away any unused medicine after the beyond-use date. Do not flush unused medications or pour down a sink or drain.
- Scanlon JEM, Chin KC, Morgan MEI, et al. Caffeine or theophylline for neonatal apnea? Arch Dis Child 1992;67:425-8.
- Kroboth PD, Slalek FS, Pittenger AL et al. DHEA and DHEA-S: a review. J Clin Pharmacol 1999;39:327-348.
- Skolnick AA. Medical news and perspectives-scientific verdict still out on DHEA. JAMA 1996;276:1365-1367.
- Kreider RB. Dietary supplements and the promotion of muscle growth with resistance exercise. Sports Med 1999;27:97-110.
- Kalra, B., Kalra, S. & Sharma, J. B. The inositols and polycystic ovary syndrome. Indian J. Endocrinol. Metab. 20, 720–724 (2016).
- Bizzarri, M., Fuso, A., Dinicola, S., Cucina, A. & Bevilacqua, A. Pharmacodynamics and pharmacokinetics of inositol(s) in health and disease. Expert Opinion on Drug Metabolism and Toxicology vol. 12 1181–1196 (2016).
- Donne, M. L. E., Metro, D., Alibrandi, A., Papa, M. & Benvenga, S. Effects of three treatment modalities (diet, myoinositol or myoinositol associated with D-chiro-inositol) on clinical and body composition outcomes in women with polycystic ovary syndrome. Eur. Rev. Med. Pharmacol. Sci. 23, 2293–2301 (2019).
- Shokrpour, M. et al. Comparison of myo-inositol and metformin on glycemic control, lipid profiles, and gene expression related to insulin and lipid metabolism in women with polycystic ovary syndrome: a randomized controlled clinical trial. Gynecol. Endocrinol. 35, 406–411 (2019).
- Effects of three treatment modalities (diet, myoinositol or myoinositol associated with D-chiro-inositol) on clinical and body composition outcomes in women with polycystic ovary syndrome.
- Martínez, Y. et al. The role of methionine on metabolism, oxidative stress, and diseases. Amino Acids vol. 49 2091–2098 (2017).
- Zhou, X. et al. Methionine restriction on lipid metabolism and its possible mechanisms. Amino Acids vol. 48 1533–1540 (2016).
- S-Adenosyl-L-Methionine (SAMe): In Depth | NCCIH. https://www.nccih.nih.gov/health/sadenosyllmethionine-same-in-depth.
- Chiang, P. K. et al. S‐Adenosylmetliionine and methylation. FASEB J. 10, 471–480 (1996).
- Obeid, R. & Herrmann, W. Homocysteine and lipids: S-Adenosyl methionine as a key intermediate. FEBS Letters vol. 583 1215–1225 (2009)
- Sharma, A. et al. S-adenosylmethionine (SAMe) for neuropsychiatric disorders: A clinician-oriented review of research. Journal of Clinical Psychiatry vol. 78 e656–e667 (2017).
- O’Connor PG, Kosten TR. Rapid and ultrarapid opioid detoxification techniques. JAMA 1998;279:229-234.
- Suprenza (phentermine hydrochloride) package insert. Cranford, NJ: Akrimax Pharmaceuticals; 2011 Oct.
- Montague DK, Jarow JP, Broderick GA, et al. Chapter 1: The management of erectile dysfunction: an AUA update. J Urol 2005;174:230-9.
- Lebret T, Herve JM, Gorny P, et al. Efficacy and safety of a novel combination of L-arginine glutamate and yohimbine hydrochloride: a new oral therapy for erectile dysfunction. Eur Urol 2002;41:608-13.
- Araneo BA, Ryu SY, Barton S, et al. Dehydroepiandrosterone reduces progressive dermal ischemia caused by thermal injury. J Surg Res 1995;59:250-262.
- Jesse Rl, Loesser K, Eich DM, et al. Dehydroepiandrosterone inhibits human platelet aggregation in vitro and in vivo. Ann N Y Acad Sci 1995;774:281-290.
- 25801
- Ortmeyer, H. K. Dietary myoinositol results in lower urine glucose and in lower postprandial plasma glucose in obese insulin resistant rhesus monkeys. Obes. Res. 4, 569–575 (1996).
- Pintaudi, B., Di Vieste, G. & Bonomo, M. The Effectiveness of Myo-Inositol and D-Chiro Inositol Treatment in Type 2 Diabetes. Int. J. Endocrinol. 2016, (2016).
- Fan, C. et al. Effects of D-Chiro-Inositol on Glucose Metabolism in db/db Mice and the Associated Underlying Mechanisms. Front. Pharmacol. 11, 354 (2020).
- Bevilacqua, A. & Bizzarri, M. Inositols in insulin signaling and glucose metabolism. International Journal of Endocrinology vol. 2018 (2018).
- Kenney, J. L. & Carlberg, K. A. The effect of choline and myo-inositol on liver and carcass fat levels in aerobically trained rats. Int. J. Sports Med. 16, 114–116 (1995).
- Andersen, D. B. & Holub, B. J. The relative response of hepatic lipids in the rat to graded levels of dietary myo-inositol and other lipotropes. J. Nutr. 110, 496–504 (1980).
- Shimada, M., Hibino, M. & Takeshita, A. Dietary supplementation with myo-inositol reduces hepatic triglyceride accumulation and expression of both fructolytic and lipogenic genes in rats fed a high-fructose diet. Nutr. Res. 47, 21–27 (2017).
- Mato, J. M., Martínez-Chantar, M. L. & Lu, S. C. S-adenosylmethionine metabolism and liver disease. Annals of Hepatology vol. 12 183–189 (2013).
- Elshorbagy, A. K. et al. S-Adenosylmethionine Is Associated with Fat Mass and Truncal Adiposity in Older Adults. J. Nutr. 143, 1982–1988 (2013).
- Yue, T., Fang, Q., Yin, J., Li, D. & Li, W. S-adenosylmethionine stimulates fatty acid metabolism-linked gene expression in porcine muscle satellite cells. Mol. Biol. Rep. 37, 3143–3149 (2010).
- Da Silva, R. P., Nissim, I., Brosnan, M. E., Brosnan, J. T. & Labrador, C. ; Creatine synthesis: hepatic metabolism of guanidinoacetate and creatine in the rat in vitro and in vivo. Am J Physiol Endocrinol Metab 296, 256–261 (2009).
- Adipex-P (phentermine hydrochloride tablets and capsules) package insert. Sellersville, PA: Teva Pharmaceuticals; 2013 Jan.
- Zolkowska D, Rothman RB, Baumann MH. Amphetamine analogs increase plasma serotonin: implications for cardiac and pulmonary disease. J Pharmacol Exp Ther. 2006;318:604-610.
- Bhatia J. Current options in the management of apnea of prematurity. Clin Pediatr 2000;39:327-36.
- Cafcit (caffeine citrate) package insert. Eatontown, NJ: West-Ward Pharmaceuticals; 2019 Dec.
- Erenberg A, Leff RD, Haack DG, et al. Caffeine Citrate for the Treatment of Apnea of Prematurity: A Double-Blind, Placebo-Controlled Study. Pharmacotherapy 2000;20(6):644–652.
- Kaltenbach T, Crockett S, Gerson LB. Are lifestyle measures effective in patients with gastroesophageal reflux disease? An evidence-based approach. Arch Intern Med. 2006;166:965-971.
- Christian MS, Brent RL. Teratogen update: evaluation of the reproductive and developmental risks of caffeine. Teratology 2001;64:51-78.
- Hadeed A, Siegel S. Newborn cardiac arrhythmias associated with maternal caffeine use during pregnancy. Clin Pediatr 1993;32:45-7.
- American Academy of Pediatrics (AAP) Committee on Drugs. Transfer of drugs and other chemicals into human milk. Pediatrics 2001;108(3):776-789.
- Le Guennec JC, Billon B. Delay in caffeine elimination in breast-fed infants. Pediatrics 1987;79:264-8.
- Berlin CM, Denson HM, Daniel CH, et al. Disposition of dietary caffeine in milk, saliva, and plasma of lactating women. Pediatrics 1984;73:59-63.
- Tyrala EE, Dodson WE. Caffeine secretion into breast milk. Arch Dis Child 1979;54:787-800.
- Hill RM, Craig JP, Chaney MD, et al. Utilization of over-the-counter drugs during pregnancy. Clin Obstet Gynecol 1977;20:381-94.
- Awake (caffeine) tablet package insert. Deerfield, IL: Walgreen Co. 05/214.
- Katz S, Morales AJ. Dehydroepiandrosterone (DHEA) and DHEA-sulfate (DS) as therapeutic options in menopause. Semin Reprod Endocrinol 1998;16:161-170.
- Rosenfield RL. Ovarian and adrenal function in polycystic ovary syndrome. Endocrinol Metab Clin North Am 1999;28:265-293.
- Wellman M, Shane-McWhorter L, Orlando PL et al. The role of dehydroepiandrosterone in diabetes mellitus. Pharmacotherapy 1999;19:582-591.
- Centurelli MA, Abate MA. The role of dehydroepiandrosterone in AIDS. Ann Pharmacother 1997;31:639-642.
- Naltrexone (naltrexone hydrochloride) package insert. Hazelwood, MO: Mallinckrodt, Inc. 2009 Feb.
- Vivitrol (naltrexone extended release injectable suspension) package insert. Cambridge, MA: Alkermes, Inc.; 2013 Aug.
- Revia (naltrexone hydrochloride) package insert. Pomona, NY: Duramed Pharmaceuticals, Inc. 2013 Oct.
- American Academy of Pediatrics (AAP) Committee on Drugs. Transfer of drugs and other chemicals into human milk. Pediatrics 2001;108:776-89.
- Adipex-P (phentermine hydrochloride tablets and capsules) package insert. Sellersville, PA: Teva Pharmaceuticals; 2013 Jan.
- Suprenza (phentermine hydrochloride) package insert. Cranford, NJ: Akrimax Pharmaceuticals; 2011 Oct.
- Phentermine hydrochloride package insert. Newtown, PA: KVK-Tech Inc; 2010 April.
- Steiner E, Villen T, Hallberg M, et al. Amphetamine secretion in breast milk. Eur J Clin Pharmacol 1984;27:123-4.
- Yocon (yohimbine hydrochloride, USP) package insert. Englewood, NJ: Glenwood, LLC; 2003, Jan.
- Vitagliano, A. et al. Inositol for the prevention of gestational diabetes: a systematic review and meta-analysis of randomized controlled trials. Archives of Gynecology and Obstetrics vol. 299 55–68 (2019).
- Isabella, R. & Raffone, E. Does ovary need D-chiro-inositol? J. Ovarian Res. 5, 1–5 (2012).
- Rees, W. D., Wilson, F. A. & Maloney, C. A. Sulfur amino acid metabolism in pregnancy: The impact of methionine in the maternal diet. in Journal of Nutrition vol. 136 1701–1705 (American Institute of Nutrition, 2006).
- Nawrot P, Jordan S, Eastwood J, et al: Effects of caffeine on human health. Food Addit Contam 2003;20:1-30.
- Schmidt B, Roberts RS, Davis P, et al. Caffeine Therapy for Apnea of Prematurity. N Engl J Med 2006; 354:2112-2121.
- lane AJ, Coombs RC, et al. Effect of caffeine on neonatal splanchnic blood flow. Arch Dis Child Fetal Neonatal Ed 1999;80:F128–F129.
- Bhatt-Mehta V, Schumacher RE. Treatment of apnea of prematurity. Pediatr Drugs 2003;5:195-210.
- Caffeine tablets alertness aid supplement (product label). Woonsocket RI, CVS; 2012.
- Pollak C, Bright D. Caffeine consumption and weekly sleep patterns in US seventh-, eighth-, and ninth-graders. Pediatrics 2003;111:42-46.
- Davis R, Osorio I: Childhood caffeine tic syndrome. Pediatrics 1998;101:E4.
- Prolab Caffeine supplement product label. Chatsworth, CA Prolab Nutrition Inc; 2012.
- VanVollenhoven RF, Engleman EG, McGuire JL. Dehydroepiandrosterone in systemic lupus erythematosus. Arthritis Rheum 1995;38:1826-1831.
- Helzlsouer KJ, Alberg AJ, Gordon GB, et al. Serum gonadotropins and steroid hormones and the development of ovarian cancer. JAMA 1995;274:1926-1930.
- Jones JA, Nguyen A, Straub M, et al. Use of DHEA in a patient with advanced prostate cancer: a case report and a review. Urology 1997;50:784-788.
- Singh, P. (2018, October 17). Methionine drug information – indications, dosage, side effects and precautions. Medindia. Retrieved June 29, 2022, from https://www.medindia.net/doctors/drug_information/methionine.htm
- Vivitrol (naltrexone extended release injectable suspension) package insert. Waltham, MA: Alkermes, Inc.; 2021 Mar.
- Suprenza (phentermine hydrochloride) package insert. Cranford, NJ: Akrimax Pharmaceuticals; 2011 Oct.
- Phentermine hydrochloride package insert. Newtown, PA: KVK-Tech Inc; 2010 April.
- Lomaira (phentermine hydrochloride) package insert. Newton, PA: KVK-Tech, Inc.; 2016 Sept.
- Hendricks EJ, Srisurapanont M, Schmidt SL, et al. Addiction potential of phentermine prescribed during long-term treatment of obesity. Int J Obes (Lond). 2014;38:292-298.
503A vs 503B
- 503A pharmacies compound products for specific patients whose prescriptions are sent by their healthcare provider.
- 503B outsourcing facilities compound products on a larger scale (bulk amounts) for healthcare providers to have on hand and administer to patients in their offices.
Frequently asked questions
Our team of experts has the answers you're looking for.
A clinical pharmacist cannot recommend a specific doctor. Because we are licensed in all 50 states*, we can accept prescriptions from many licensed prescribers if the prescription is written within their scope of practice and with a valid patient-practitioner relationship.
*Licensing is subject to change.
Each injectable IV product will have the osmolarity listed on the label located on the vial.
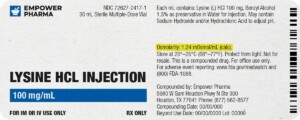
Given the vastness and uniqueness of individualized compounded formulations, it is impossible to list every potential compound we offer. To inquire if we currently carry or can compound your prescription, please fill out the form located on our Contact page or call us at (877) 562-8577.
We source all our medications and active pharmaceutical ingredients from FDA-registered suppliers and manufacturers.
We're licensed to ship nationwide.
We ship orders directly to you, quickly and discreetly.
 Metformin Synergy Capsules
Metformin Synergy Capsules Lisinopril Tablets
Lisinopril Tablets Lipo Injection
Lipo Injection Phentermine HCl / Topiramate Capsules
Phentermine HCl / Topiramate Capsules Phendimetrazine Tartrate Tablets
Phendimetrazine Tartrate Tablets Bupropion HCl SR Tablets
Bupropion HCl SR Tablets 7-Keto DHEA Capsules
7-Keto DHEA Capsules Bella Capsules
Bella Capsules Methylcobalamin Injection (Vitamin B12)
Methylcobalamin Injection (Vitamin B12) Metformin Tablets
Metformin Tablets